Print Friendly
Special Considerations in Diagnosing and Treating ADHD
Part 3: Adults
Sharon Wigal, PhD
Clinical Professor of Pediatrics, University of California, Irvine
Timothy Wigal, PhD
Associate Clinical Professor of Pediatrics, University
of California, Irvine
This CME activity is now expired. Please visit www.psychiatryweekly.com to view current activities.
This is the third in a 3-part Psychiatry Weekly CME series on special considerations in diagnosing and treating
ADHD. Parts 1 and 2 focused
on the preschool-age population, and the child and adolescent population, respectively.
Accreditation Statement

This activity has been planned and implemented in accordance with the Essentials and Standards of the Accreditation Council
for Continuing Medical Education (ACCME) through the joint sponsorship of the Mount Sinai School of Medicine and MBL Communications,
Inc. The Mount Sinai School of Medicine is accredited by the ACCME to provide continuing medical education for physicians.
Credit Designation
The Mount Sinai School of Medicine designates this educational activity for a maximum of 1 AMA PRA Category 1 Credit(s)TM.
Physicians should only claim credit commensurate with the extent of their participation in the activity.
Faculty Disclosure Policy Statement
It is the policy of the Mount Sinai School of Medicine to ensure objectivity, balance, independence, transparency, and
scientific rigor in all CME-sponsored educational activities. All faculty participating in the planning or implementation
of a sponsored activity are expected to disclose to the audience any relevant financial relationships and to assist in
resolving any conflict of interest that may arise from the relationship. Presenters must also make a meaningful disclosure
to the audience of their discussions of unlabeled or unapproved drugs or devices.
This activity has been peer reviewed and approved by Eric Hollander, MD, Professor of Psychiatry and Chair at Mount Sinai
School of Medicine. Review Date: May 31, 2007
Statement of Need
6%–9% of children are estimated to have ADHD, and 65%–85% of children with ADHD continue to meet at least
some criteria for ADHD and present with significant impairment as adults. Of the estimated 4%–5% of adults with ADHD,
only 20% are ever diagnosed. Recognition in this patient population is complicated by the dominance of inattentive symptoms
(which are less likely to draw notice than hyperactive symptoms). Diagnosis is complicated both by the difficulty of obtaining
reliable information on symptoms from early childhood, and the high prevalence of comorbidities.
Common comorbidities include substance abuse, mood disorders, and anxiety disorders, all of which significantly impact
a patient’s quality of life and can contribute to the overall impairment of adults with ADHD, who earn less money,
experience more difficulty at work, and change jobs more often than adults without ADHD. Psychosocial and pharmacologic
treatment are both used, and the latter is predominantly stimulants, though one non-stimulant medication has been FDA approved
for this patient population.
An important educational need exists to refine the diagnostic and treatment strategies of clinicians treating adult patients
with ADHD. Particularly in light of the significant impairment caused by ADHD, effort must be made to increase recognition
among this patient population. Clinicians must also keep abreast of emerging data on treatment efficacy.
Learning Objectives
- Describe the impact of ADHD in the adult population, and the role of comorbid disorders in diagnosis, impairment, and
treatment response.
- Assess treatment options for adults with ADHD.
- Explain the difficulties in diagnosing this patient population, and be aware
of diagnostic strategies designed to counter these difficulties.
Target Audience
This activity will benefit psychiatrists, hospital staff physicians, and office-based “attending” physicians
from the community.
Funding/Support
This activity is supported by an educational grant from Shire.
Faculty Disclosures
Sharon Wigal, PhD, has disclosed that she has received research support from Cephalon, Eli Lilly, McNeil,
New Rivers, NIH, and Shire; has served as an advisor or consultant to Cephalon, McNeil, New Rivers, Novartis, Shire, and
UCB; and has served on the speaker’s bureau for McNeil, Shire, and UCB.
Timothy Wigal, PhD, has disclosed that he has received research support from Cephalon, Eli Lilly, McNeil,
New Rivers, NIH, Novartis, and Shire; has served as a consultant or advisor to McNeil, Novartis, and Shire; and has served
on the speaker’s bureau of McNeil and Shire.
Peer Reviewers
Eric Hollander, MD, reports no affiliation with or financial interest in any organization that may pose
a conflict of interest
Daniel Stewart, MD, PhD, reports no affiliation with or financial interest in any organization that may
pose a conflict of interest.
To Receive Credit for this Activity
Read this poster, reflect on the information presented, and then complete the CME quiz found in the accompanying brochure
or online (www.mssmtv.org/psychweekly). To obtain credit you should score 70% or better. The estimated time to complete this
activity is 1 hour.
Release Date: July 9, 2007
Termination Date: July 9, 2009
Introduction/Prevalence
65%-85% of children with ADHD continue to meet at least some of the criteria for ADHD and present with impairment related
to primary symptoms of the disorder as adults.1 Evidence indicates that 4%-5% of adults have ADHD and that <20%
of them are diagnosed.2 Presentation in adults is heavily biased toward inattentive symptoms,3 which
are less likely to draw notice than hyperactive or impulsive symptoms and may contribute to the under-recognition of ADHD
in this patient population. Diagnosis is complicated both by the necessity of demonstrating symptom onset prior to 7 years
of age and by the prevalence of comorbid psychiatric disorders in adults with ADHD; anxiety disorders and substance abuse
are particularly prevalent in this population.4 Identifying comorbid disorders in ADHD is particularly important
as they can interfere with diagnosis and complicate treatment. Symptoms of ADHD can severely impact an adult’s life;
the disorder is implicated in more frequent job changes, more martial discord, and decreased quality of life.
Presentation and Impact
Male children are far more
likely to be diagnosed with ADHD than female children; by late adolescence and
adulthood the ratio has shrunk from 3:1 to 1:1.6,7 This may be due
to the predominance of hyperactivity in male children with ADHD and the
diminution of hyperactive symptoms across individuals with ADHD as they age
(hyperactive symptoms are generally easier to spot than inattentive symptoms).
ADHD may manifest differently in females than males, but more research is
needed to clarify gender-related issues in diagnosis, treatment, and the impact
of ADHD symptoms on life events. Adult males with ADHD earn less money,
experience more difficulty at work, and change jobs more often than adult males
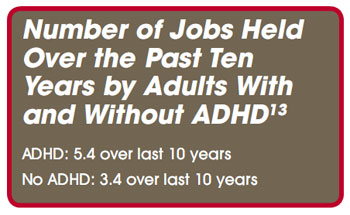
without ADHD.8 Adults diagnosed with ADHD also have, on average,
fewer years of education and are less likely to be professionally employed.9
 Other studies have indicated
that patients with substance use disorders and ADHD are more prone to social
maladjustment, lower levels of work-related achievement, and higher rates of
separation and divorce than are patients with substance use disorders without
comorbid ADHD.10,11 There is also evidence that adults with ADHD are
more likely to report psychological maladjustment and to have more speeding
violations than adults without ADHD.12 Adults with ADHD also report
less satisfaction in the workplace and in life in general.13
Other studies have indicated
that patients with substance use disorders and ADHD are more prone to social
maladjustment, lower levels of work-related achievement, and higher rates of
separation and divorce than are patients with substance use disorders without
comorbid ADHD.10,11 There is also evidence that adults with ADHD are
more likely to report psychological maladjustment and to have more speeding
violations than adults without ADHD.12 Adults with ADHD also report
less satisfaction in the workplace and in life in general.13
Adults
with ADHD may have developed effective coping skills over the years, but they
tend to have difficulty with time management, sleeping, motivation, and tolerating
frustration. They are also prone to talking too much and/or too fast at work
and in social situations. They are likely to seek help when managing the
demands of work and/or home life become overwhelming.14-16
Comorbidity
Comorbid disorders are
common in adults with ADHD. Anxiety disorders, substance abuse disorders, and
mood disorders are all highly prevalent comorbidities in this patient
population, and there is also a significant incidence of antisocial disorder.
Substance Use Disorders
Substance
use disorders tend to manifest in adolescence or early adulthood and affect
15%-20% of adults in the US.20 There is significant bi-directional
overlap between ADHD and substance-use disorders; 40%-50% of adults with ADHD
present with comorbid substance abuse, and 15%-25% of adults with substance use
disorders present with comorbid ADHD. Marijuana is the most common substance
abused by adults with ADHD, although alcohol abuse is also common.21
Substance
use disorders have a significant impact on the long-term course of ADHD; not
only are patients with ADHD and comorbid substance abuse more likely to have
another psychiatric disorder, but patients with ADHD and comorbid substance
abuse have been found to have an earlier onset of symptoms, longer course and
greater severity of disease, and more relapses. ADHD has also been linked with
increased risk of cigarette use and increased difficulty in quitting smoking.21
The latter may be due in part to nicotine’s reducing ADHD symptoms.22 Early
treatment with stimulants may decrease the risk for later development of
substance use disorders, particularly when adolescents maintain pharmacotherapy.23
First-line treatment for adults with ADHD and recently resolved substance abuse
may include atomoxetine or strongly noradrenergic TCAs, due to their lack of a
dopaminergic effect, and stimulants with decreased liability for abuse.24
Depression
Up to
50% of adults with ADHD will experience at least one depressive episode during
their lifetime,25 with up to 35% suffering from major depression.26
There is evidence that patients with comorbid ADHD and depression respond well
to antidepressants but do not respond as well to treatments for ADHD as do
patients with ADHD without comorbid depression.27 Thus, clinicians
may consider attempting to treat the depression before prescribing stimulants
in patients with comorbid ADHD and depression.28 If treating both
disorders simultaneously, MAOIs must not be prescribed with stimulants due to
the possibility of hypertensive crisis.29 Overall, practitioners
must exercise caution when prescribing stimulants and TCAs in combination due
to the product labeling contraindication, although research suggests the
combination is generally safe.30
Bipolar Disorder
Approximately
10%-15% of adults with ADHD co-present with bipolar disorder, and males are
more likely than females to present with both disorders. The disorders are
further linked in that the onset of mood disorder in patients with comorbid
ADHD and bipolar disorder predates the onset of mood disorder in patients
without ADHD by an average of 5 years. Comorbid ADHD and bipolar
disorder have also been linked to increased severity of bipolar disorder.31
Other Comorbid Disorders
Comorbid
anxiety disorder is highly prevalent in adults with ADHD, but evidence of the
interaction of anxiety with ADHD is unclear. There is some indication that
adults with comorbid ADHD and an anxiety disorder have more pronounced
attentional deficits.31 In addition, studies have shown that ADHD in
adults is strongly associated with sleep disturbance,32 but it is
not clear whether actual sleep disorders are linked with adult ADHD. Poor sleep
patterns contribute to a worsening of ADHD symptoms in adults, and stimulant
treatment has been shown to improve overall sleep.33 Personality
disorders co-present in 10%-15% of adults with ADHD, and children with ADHD are
far more likely to have an antisocial personality disorder as an adult.34
Diagnosis
Numerous
obstacles beset diagnosis of ADHD in adults. The DSM-IV criteria are
geared toward school-age children, yet ADHD persists into adolescence and
adulthood and may not be diagnosed until the adult years.35 Further,
diagnosis of ADHD in adults requires marshalling evidence that the symptoms
began before the age of 7 years old. Self-reports are flawed; aside from
obvious difficulties centered around recalling symptoms that occurred many
years ago,36 adults have been shown to deny symptoms that are
verified by others.37 Difficulty with diagnosis of ADHD in adults is
further compounded by the fact that hyperactive symptoms, which are generally
the easiest symptoms to observe in an interview setting, usually decline with
age. Unlike children, most adults with ADHD have the freedom to avoid overly
structured situations, and a strong base of support at home or at work can make
it difficult to identify substantial impairment in multiple settings. Finally,
the high rate of symptom overlap between comorbid psychiatric disorders in
adults with ADHD impedes diagnosis. Impulsivity, for example, is a defining
symptom of both bipolar disorder and ADHD, while poor concentration is common
in both depression and ADHD.
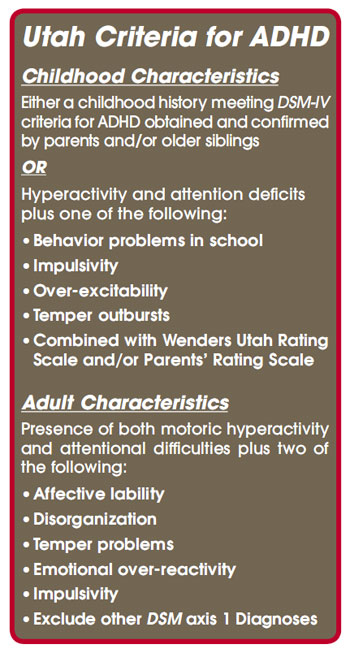
In
order to address the difficulties of retrospectively identifying childhood symptoms,
researchers at the University of Utah School of Medicine Department of Psychiatry
have developed a set of criteria for diagnosing ADHD in adults.38
The Utah Criteria eschew specific cataloguing of childhood symptoms, focusing
instead on recollection of problem areas that may be more easily recalled by
the patient or a parent or former teacher (eg, behavior problems in school).
The Utah Criteria may result in a more inclusionary diagnosis than strictly
following the DSM-IV criteria, and this could, in turn, result in
identifying patients who would benefit from treatment despite not meeting
formal diagnostic criteria.39
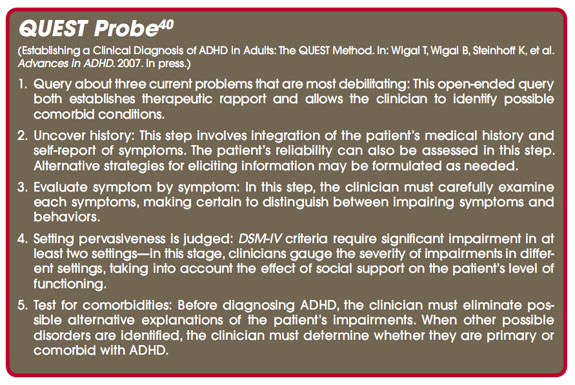
Recently,
investigators at the University of California, Irvine, Child Development Center
have developed a method of more effectively diagnosing ADHD in adults. Called
“QUEST,’ the method is geared toward identifying the problematic behaviors in
adults with age-appropriate probes combined with a logical, careful approach.
- Query about three current problems that are most debilitating:
This open-ended query both establishes therapeutic rapport and allows the
clinician to identify possible comorbid conditions.
- Uncover history: This step involves integration of the patient’s medical history and self-report
of symptoms. The patient’s reliability can also be assessed in this step. Alternative
strategies for eliciting information may be formulated as needed.
- Evaluate symptom by symptom: In this step, the clinician must carefully
examine each symptoms, making certain to distinguish between impairing symptoms
and behaviors.
- Setting pervasiveness is judged: DSM-IV criteria
require significant impairment in at least two settings—in this stage,
clinicians gauge the severity of impairments in different settings, taking into
account the effect of social support on the patient’s level of functioning.
- Test for comorbidities: Before diagnosing ADHD, the
clinician must eliminate possible alternative explanations of the patient’s
impairments. When other possible disorders are identified, the clinician must
determine whether they are primary or comorbid with ADHD.
Management
Management of adult ADHD
should involve both psychosocial and pharmacologic treatment. Counseling and
patient education is recommended,39 and evidence suggests that
cognitive behavioral therapy in conjunction with pharmacotherapy outperforms
pharmacotherapy alone.41
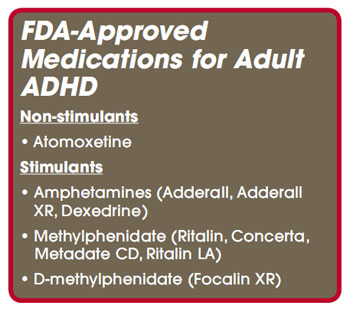
Atomoxetine
was the first medication approved by the FDA for treating adults with ADHD, and
it currently is the only non-stimulant medication with this labeled indication.
Atomoxetine, a selective norepinephrine reuptake inhibitor, shows limited
clinical efficacy in adults, but a number of studies indicate it has promise
particularly for some patients.42,43
The
FOCUS (Formal Observation of Concerta versus Strattera) study, published in
2005, indicated that, while both methylphenidate and atomoxetine are effective
treatments for ADHD, methylphenidate is associated with significantly greater
symptom improvement.44 Because atomoxetine is not a Schedule II
medication, practitioners may be more inclined to prescribe it for patients
with a history of substance abuse or tic disorders.45,46
However, atomoxetine use produces a number of side effects including dry mouth, insomnia, nausea, and erectile difficulty.45,46
Blood pressure should also be monitored in patients taking this medication.47
Psychostimulants
are first-line treatments for ADHD due to their established efficacy and
safety. Methylphenidate (MPH) has been shown to be effective in adults48
and is now available in an FDA-approved extended-release formulation.
Amphetamines are similarly effective as MPH, and are often prescribed as a
second-line treatment when MPH is not well-tolerated or does not lead to optimal
efficacy.49 D-methylphenidate functions similarly to MPH, but only
half the dose size is required and it may have an altered side-effect profile.50
Adverse events most commonly observed with stimulant treatment are headache,
abdominal pain, jitteriness, decreased appetite, delayed sleep onset, social
withdrawal, and loss of appetite, and dry mouth has been reported in adults in
particular.51
References
1.
Biederman J, Monuteaux M, Mick E, et al. Young adult outcome of attention deficit hyperactivity disorder: a controlled 10
year follow-up study. Psychol Med. 2006;36:167-179.
2.
Kessler RC, Adler L, Barkle R, et al. the prevalence and correlates of adult ADHD in the United States: results from the
National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
3.
Milstein RB, Wilens TE, Biederman J, et al. Presenting ADHD symptoms and subtypes in clinically referred adults with ADHD. J
Atten Disord. 1997;2:159-166.
4.
McGough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder:
findings from multiplex families. Am J Psychiatry. 2005;162:1621-1627.
5.
Biederman J, Faraone SV, Spencer T, et al. Functional impairments in adults with self-reports of diagnosed ADHD: a controlled
study of 1001 adults in the community. J Clin Psychiatry. 2006;67:524:540.
6.
Kessler RC, Adler L, Barkley R, et al. The prevalence and correlates of adult ADHD in the United States: results from the
National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
7.
Faraone SV, Sergeant J, Gillberg C, et al. The worldwide prevalence of ADHD: is it an American condition? World Psychiatry.
2003;163:716-723.
8.
Borland BL, Heckman HK. Hyperactive boys and their brothers: a 25-year follow-up study. Arch Gen Psychiatry. 1976;33:669-675.
9.
Morrison JR. Childhood hyperactivity in an adult psychiatric population: social factors. J Clin Psychiatry. 1980;41:40-43.
10.
Wilens TE, Biederman J, Mick E. Does ADHD affect the course of substance abuse? Findings from a sample of adults with and
without ADHD. Am J Addict. 1998;7:156-163.
11.
Tarter RE. Psychosocial history, minimal brain dysfunction and differential drinking patterns of male alcoholics. J
Clin Psychol. 1982;38:867-873.
12.
Murphy K, Barkley RA. Attention deficit hyperactivity disorder adults comorbidities and adaptive impairments. Compr
Psychiatry. 1996;37:393-401.
13.
Biederman J, Faraone SV, Spencer T, et al. Functional impairments in adults with self-reports of diagnosed ADHD: A controlled
study of 1001 adults in the community. J Clin Psychiatry. 2006;67:524-540.
14.
Barkley RA, Fischer M, Fletcher K, et al. Persistence of attention deficit hyperactivity disorder into adulthood as a function
of reporting source and definition of disorder. J Abnorm Psychol. 2002;111:279-289.
15.
Weiss M, Murray C. Assessment and management of attention-deficit hyperactivity disorder in adults. CMAJ. 2003;168:715-722.
16.
Barkley RA. Major life activity and health outcomes associated with attention deficit/hyperactivity disorder. J Clin
Psychiatry. 2002;63(Suppl 12):10-15.
17.
Shekin WO, Asarnow RF, Hess E, et al. A clinical and demographic profile of a sample of adults with attention deficit hyperactivity
disorder, residual state. Compr Psychiatry. 1990;31:416-425.
18.
Biederman J, Faraone SV, Spencer T, et al. Patterns of psychiatric comoribidty, cognition, and psychosocial funcitioning
in adults with attention deficit hyperactivity disorder. Am J Psychiatry. 1993;150:1792-1798.
19.
Mcough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder:
findings from multiplex families. Am J Psychiatry. 2005;162:1621-1627.
20.
Kessler RC, Berglund P, Demler O, Jin R, Merikangas KR, Walters EE. Lifetime prevalence and age-of-onset distributions
DSM-IV disorders in the national Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593-602.
21.
Wilens TE. Attention-deficit/hyperactivity disorder and the substance use disorders: the nature of the relationship, subtypes
at risk, and treatment issues. Psychiatr Clin North Am. 2004;27:283-301.
22.
Rush CR, Higgins ST, Vansickel AR, Stoops WW, Lile JA, Glaser PE. Methylphenidate increases cigarette smoking. Psychopharmacology
(Berl). 2005;181:781-789.
23.
Wilens TE, Faraone SV, Biederman J, Gunawardene S. Does stimulant therapy of attention-deficit/hyperactivity disorder beget
later substance abuse? A meta-analytic review of the literature. Pediatrics. 2003;11:179-185.
24.
Sobanski E. Pschiatric comorbidity in adults with attention-deficity/hyperactivity disorder (ADHD). Eur Arch Psychiatry
Clin Neurosci. 2006;256:26-31.
25.
Kessler RC, Adler L, Barkle R, et al. the prevalence and correlates of adult ADHD in the United States: results from the
National Comorbidity Survey Replication. Am J Psychiatry. 2006;163:716-723.
26.
Mcough JJ, Smalley SL, McCracken JT, et al. Psychiatric comorbidity in adult attention deficit hyperactivity disorder:
findings from multiplex families. Am J Psychiatry. 2005;162:1621-1627.
27.
Wender PH, Reimherr FW, Wood D, Ward M. A controlled study of methylphenidate in the treatment of attention deficit disorder,
residual type, in adults. Am J Psychiatry. 1985:142:547-552.
28.
Sobanski E. Psychiatric comorbidity in adults with attention-deficity/hyperactivity disorder (ADHD). Eur Arch Psychiatry
Clin Neurosci. 2006;256:26-31.
29.
Markowitz JS. Drug interactions with stimulant medications. Int Clin Psychopharmacol. 1999;14:1-18.
30.
Greenhill LL, Pliszka S, Dulcan MK, et al. Practice parameter for the use of stimulant mediaction in the treatment of children,
adolescents and adults. J Am Acad Child Adolesc Psychiatry. 2002;41:26S-49S.
31.
Nierenberg AA, Mihahara S, Spencer T, et al. Clinical and diagnostic implications of lifetime comorbidity of attention-deficit/hyperactivity
disorder in adults with bipolar disorder.Data from the first 1000 STEP-BD participants. Biol Psychiatry. 2005:57;1467-1473.
32.
Brown TE, McMullen WJ. Attention deficit disorders and sleep/arousal disturbance. Ann NY Acad Sci. 2001;931:271-286.
33.
Kooj JJS, Huub AM, Middelkoop AM, Van Gils K, Buitelaar JK. The effect of stimulants on nocturnal activity and sleep quality
in adults with ADHD: an open-label case-control study. J Clin Psychiatry. 2001;62:952-955.
34.
Manuzza S, Klein RG, Bessler A, Malloy P, La Padula M. Adult outcome of hyperactive boys. Educational achievement, occupational
rank, and psychiatric status. Arch Gen Psychiatry. 1993;50:565-567.
35.
Diagnostic and Statistical Manual of Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association; 1994.
36.
Faraone SV, Biederman J, Doyle A, et al. Neuropsychological Studies of Late Onset and Subthreshhold Diagnoses of Adult
Attention-Deficit/Hyperactivity Disorder. Biol Psychiatry. 2006;60:1081-1087.
37.
Ward MF, Wender PH, Reimherr FW. The Wender Utah Rating Scale: an aid in the retrospective diagnosis of childhood attention
deficit hyperactivity disorder. Am J Psychiatry. 1993;150:885-890.
38.
Wender PH. Attention-Deficit Hyperactivity Disorder in Adults. New York, NY: Oxford University Press; 1995.
39.
Ginsberg D, Donnely C, Reimherr F, Young J. Differential diagnosis and treatment of adult ADHD and neighboring disorders. CNS
Spectr. 2006;10(Suppl 11):1-16.
40.
Establishing a Clinical Diagnosis of ADHD in Adults: The QUEST Method. Wigal T, Wigal B, Steinhoff K, et al. Advances
in ADHD. 2007. In press.
41.
Safren SA, Otto MW, Sprich S, Winett CL, Wilens TE, Biederman J. Cognitive-behavioral therapy for ADHD in medication-treated
adults with continued symptoms. Behav Res Ther. 2005;43:831-842.
42.
Adler LA, Spencer TJ, Milton DR, et al. Long-term, open-label study of the safety and efficacy of atomoxetine in adults
with attention-deficit/hyperactivity disorder: an interim analysis. J Clin Psychiatry. 2005;66:294-299.
43.
Michelson D, Adler L, Spencer T, et al. Atomoxetine in adults with ADHD: two randomized, placebo-controlled trials. Biol
Psychiatry. 2003;53:112-120.
44.
Starr HL, Kemner J. Multicenter, randomized, open-label study of OROS methylphenidate versus atomoxetine: treatment outcomes
in African-American children with ADHD. J Natl Med Assoc. 2005;97:11S-16S.
45.
Wilens TE. Impact of ADHD and its treatment on substance abuse in adults. J Clin Psychiatry. 2004;65(Suppl 3);38-45.
46.
Allen AJ, Kurlan RM, Gilbert DL, et al. Atomoxetine treatment in children and adolescents with ADHD and comorbid tic disorders. Neurology.
2005;65:1941-1949.
47.
Nissen SE. ADHD and cardiovascular risk. N Engl J Med. 2006;354:1445-1448.
48.
Spencer T, Biederman J, Wilens T, et al. A large, double-blind, randomized clinical trial of methylphenidate in the treatment
of adults with attention-deficit/hyperactivity disorder. Biol Psychiatry. 2005;57:456-463.
49.
Wender EH. Managing stimulant medication for attention-deficit/hyperactivity disorder. Pediatr Rev. 2001;22:183-189.
50. Dexmethylphenidate (Focalin) for ADHD. Med Lett. 2002;44:45-46.
51.
Graydanus DE, Sloane MA, Rappley MD. Psychopharmacology of ADHD in adolescents. Adolesc Med. 2002;3:599-624.