Click here to go to the CME post-test
Print Friendly
Special Considerations in Diagnosing and Treating ADHD
Part 1: Preschool-Age Children


Sharon Wigal, PhD
Clinical Professor of Pediatrics, University of California, Irvine
Timothy Wigal, PhD
Associate Clinical Professor of Pediatrics, University of California, Irvine
This is the first in a 3-part Psychiatry Weekly CME series on special considerations in diagnosing and treating
ADHD. Parts 2 and 3 in
this CME series will focus on the adolescent and adult populations respectively.
Accreditation Statement
 This
activity has been planned and implemented in accordance with the Essentials and Standards of the Accreditation Council
for Continuing Medical Education (ACCME) through the joint sponsorship of the Mount Sinai School of Medicine and MBL Communications,
Inc. The Mount Sinai School of Medicine is accredited by the ACCME to provide continuing medical education for physicians.
This
activity has been planned and implemented in accordance with the Essentials and Standards of the Accreditation Council
for Continuing Medical Education (ACCME) through the joint sponsorship of the Mount Sinai School of Medicine and MBL Communications,
Inc. The Mount Sinai School of Medicine is accredited by the ACCME to provide continuing medical education for physicians.
Credit Designation
The Mount Sinai School of Medicine designates this educational activity for a maximum of 1 AMA PRA Category 1 Credit(s)TM.
Physicians should only claim credit commensurate with the extent of their participation in the activity.
Faculty Disclosure Policy Statement
It is the policy of the Mount Sinai School of Medicine to ensure objectivity, balance, independence, transparency, and
scientific rigor in all CME-sponsored educational activities. All faculty participating in the planning or implementation
of a sponsored activity are expected to disclose to the audience any relevant financial relationships and to assist in
resolving any conflict of interest that may arise from the relationship. Presenters must also make a meaningful disclosure
to the audience of their discussions of unlabeled or unapproved drugs or devices.
This activity has been peer reviewed and approved by Eric Hollander, MD, Professor of Psychiatry and Chair at Mount Sinai
School of Medicine. Review Date: March 28, 2007.
Statement of Need
An estimated 6%–9% of children are affected by attention-deficit/hyperactivity disorder (ADHD). The diagnosis of
ADHD involves clinical evaluation of inattentive, impulsive, and hyperactive symptoms. Diagnosis of preschool age children
presents a number of unique difficulties hinging around distinguishing symptoms from natural childhood exuberance and inattention.
Treatment in this patient population has not been well-researched. Amphetamines are the only agents approved by the FDA
for the treatment of ADHD in children between the ages of 3 and 6 years at this time, but off-label methylphenidate is
the most commonly prescribed psychotropic medication for this population. Behavioral interventions have also shown promise.
An important educational need exists to refine the diagnostic and treatment strategies of clinicians in order to more
safely and effectively treat preschool-age children with ADHD. Early, accurate diagnosis is paramount, and clinicians must
remain aware of the newest information on treatment options, both pharmacotherapeutic and behavioral, available to treat
this patient population.
Learning Objectives
- Describe the importance of early and accurate diagnosis of preschool-age patients with ADHD and how comorbidity
may result in misdiagnosis.
- Assess available treatments, both off- and on-label, for safety and efficacy in preschool-age children
with ADHD.
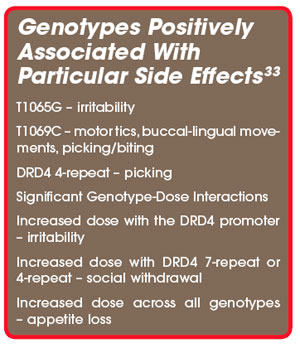
- Explain the latest information on the genetics and etiology of ADHD in preschool-age children and understand
how this affects treatment response and side effect profiles.
Target Audience
This activity will benefit psychiatrists, hospital staff physicians, and office-based “attending” physicians
from the community.
Funding/Support
This activity is supported by an educational grant from Shire.
Faculty Disclosures
Sharon Wigal, PhD, has disclosed that she has received research support from Cephalon, Eli Lilly, McNeil,
New Rivers, NIH, and Shire; has served as an advisor or consultant to Cephalon, McNeil, New Rivers, Novartis, Shire, and
UCB; and has served on the speaker’s bureau for McNeil, Shire, and UCB.
Timothy Wigal, PhD, has disclosed that he has received research support from Cephalon, Eli Lilly, McNeil,
New Rivers, NIH, Novartis, and Shire; has served as a consultant or advisor to McNeil, Novartis, and Shire; and has served
on the speaker’s bureau of McNeil and Shire.
Peer Reviewers
Eric Hollander, MD, reports no affiliation with or financial interest in any organization that may pose
a conflict of interest
Daniel Stewart, MD, PhD, reports no affiliation with or financial interest in any organization that may
pose a conflict of interest.
To Receive Credit for this Activity
Read this poster, reflect on the information presented, and then complete the CME quiz found in the accompanying brochure
or online (www.mssmtv.org/psychweekly). To obtain credit you should score 70% or better. The estimated time to complete this
activity is 1 hour.
Release Date: April 23, 2007
Termination Date: April 23, 2009
Introduction
While the literature on ADHD in
preschool-age children is limited, and the validity of the diagnosis in
children this age is contested, current prevalence estimates for this
population range between two and five percent.1 In addition, there
is substantial evidence linking ADHD symptoms in preschool-age children with
significant concomitant functional impairment and behavioral problems in later
childhood.2-8 Treatments utilized by clinicians for this population
include psychosocial treatment and the prescription of stimulants. While
methylphenidate (MPH) is the most widely used stimulant medication for treating
preschool children, MPH is not FDA-approved for use in children under the age
of 6, and few studies have examined stimulants in this population.9-10
In addition, a relatively recent study reported a 49% increase in their prescription
to children under the age of 5.9 The tentatively favorable findings
of one large NIMH-funded study on the safety and efficacy of MPH—the Preschool
ADHD Treatment Study (PATS)—were recently published in the Journal of the
American Academy of Child & Adolescent Psychiatry (2006), but the
authors noted that follow-up research was imperative.
The
lack of literature on ADHD in preschool-age children in combination with the
confusion surrounding reliable diagnosis, apparent prevalence of the disorder,
and the associated significant impairments indicate a clear and pressing need
for increased study of ADHD and ADHD-like behaviors in young children and
merits a revisiting of current best understanding and practice.
Diagnosis
A diagnosis of ADHD by DSM-IV
criteria may be classified in three ways: predominately inattentive,
predominately hyperactive-impulsive, and combined-type (both inattentive and
hyperactive-impulsive).
The
application of these criteria to young children poses problems particular to
the age group; not only is it difficult to identify inattentiveness
inconsistent with age level in preschoolers—who are, in general, far more
inattentive than older children—but it is equally difficult to identify hyperactivity-impulsivity
inconsistent with age level in this population. In essence, a certain degree of
inattentiveness and hyperactivity are the developmental standard for young
children. The key is in assessing whether the symptoms are maladaptive.
However, identifying maladaptive inattentiveness in preschool-age children is
further complicated by the fact that young children are seldom in situations
where they are asked to sustain attention. Indeed, a lack of sustained
attention is seldom maladaptive for this population—impairment is most likely
to be associated with hyperactivity.
Because ADHD is more likely to
negatively affect functioning at school, teachers are often the first to notice
a problem. The shift in preschool away from, essentially, group daycare toward
a more structured learning environment has likely contributed to the
identification of maladaptive hyperactivity, due to its disruptive nature in a
classroom setting, as well as, to a lesser extent, maladaptive inattentiveness
(again, if one is not asking a child to attend, inattentiveness will tend to go
unnoticed). Conversely, evidence suggests that parents with a child who does
meet criteria for ADHD are significantly more likely to consider hyperactivity
and inattentiveness as developmentally standard in comparison to parents whose
children do not meet criteria for ADHD.11
In
assessing a child who may have ADHD, a clinician needs to first rule out
alternative explanations for the ADHD-like symptoms. These can include, but are
by no means limited to significant life change (eg, parents’ divorce), learning
disability, a mood or anxiety disorder, and/or seizures and other medical
disorders that affect brain functioning. (NIMH ADHD site) A
thorough history, including school and medical records, and an examination of the home and classroom environment should be
the foundation of an ADHD diagnosis. The child’s teachers can be an invaluable
source of information—although generally not trained mental health
professionals, their access to comparator children (as generally opposed to a
parent’s access to same) lends significant credence to their (ie, the
teachers’) subjective measures of a child’s behavior.
Due
to the natural hyperactivity and inattentiveness of young children, a clinician
must be confident that these symptoms cause impairment to make an ADHD
diagnosis in this population.
Etiology
Over
the years, many theories regarding the cause of ADHD have been advanced, some
with more credence than others. Two views that have not withstood scientific scrutiny
are the theories that poor parenting or exposure to certain food additives
cause the disorder. Little evidence for either has been found, although diet
restriction may have a positive effect on ADHD symptoms in some young children
with food allergies.12 A positive correlation has been found between
alcohol and cigarette use during pregnancy. (NIMH
ADHD site)
There
is strong evidence for a genetic element to ADHD from both family and twin
studies.13-14 ADHD has been found to be five times more common in
the close relatives of those with ADHD than in the general population. Research
has identified genes involved in dopamine regulation, but ADHD does not appear
to be a “one-gene” disorder. Variants in the dopamine D4 receptor gene,
the dopamine DRD5 gene, and a dopamine transporter gene have all been linked
with susceptibility to ADHD.15-17
A number of
other genes have been associated with the developmental course of the disorder,
including the DRD4 7-repeat risk allele (influences persistence and antisocial
behavior), a functional variant in the gene encoding COMT (associated with
antisocial behavior in ADHD), and a variant in MAOA (associated with antisocial
behavior in ADHD).18-21
Common Comorbidities
Comorbidities
are highly prevalent in ADHD (up to 50% of children with ADHD have at least one
comorbid disorder).22 Comorbidities are more commonly identified in
older children and adults with ADHD than in preschool children; this may be
due, in part, to later emergence of certain psychiatric disorders, but is
likely also partly accounted for by the difficulty of diagnosing psychiatric
disorders in young children.
20%–30%
of children with ADHD have a specific learning disability.23 Conduct
disorders, particularly oppositional defiant disorder, are also common
comorbidities (they’re present in up to 50% of children with ADHD, though
oppositional defiant disorder predominately presents in boys). Anxiety and
depression also co-present with ADHD. Some suspect bipolar disorder is also a
common comorbidity, but there are no agreed-upon prevalence 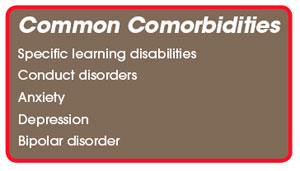 rates. In part,
this is because bipolar disorder is difficult to diagnose in children. However,
the picture is further complicated in that bipolar disorder appears to present
in children as a chronic mood dysregulation (without the cycling so important
to an adult diagnosis), making the symptoms very similar to those of ADHD.
Elated mood and grandiosity, however, are particular to children with bipolar
disorder, and can form the basis for a distinction.24
rates. In part,
this is because bipolar disorder is difficult to diagnose in children. However,
the picture is further complicated in that bipolar disorder appears to present
in children as a chronic mood dysregulation (without the cycling so important
to an adult diagnosis), making the symptoms very similar to those of ADHD.
Elated mood and grandiosity, however, are particular to children with bipolar
disorder, and can form the basis for a distinction.24
In very young
children, ADHD also shares a similar symptom cluster with autism. The similarity
of ADHD symptoms and the symptoms of other psychiatric disorders in very young
children, coupled with the difficulty of diagnosing preschool-age children, has
likely led to instances of both under and over-diagnosis of ADHD in this
patient population.
Treatment
Amphetamines (ie,
dextroamphetamine and mixed amphetamine salts) are the only agents approved by
the FDA for the treatment of ADHD in children between the ages of 3 and 6 years
at this time. Although MPH is not approved for children under 6 years of age,
it is the most commonly prescribed psychotropic medication for ADHD patients in
this population. In response to increased off-label prescription of stimulants
for preschool-age children, the National Institute of Health Consensus
Development Conference on the Diagnosis and Treatment of ADHD (1998) found a
need for further study on the safety and efficacy of stimulant medications in
young children with ADHD. Specifically, researchers stressed the need for a
better understanding of age-related effects on drug absorption and metabolism,
dose-response characteristics, and side effects of using stimulants in
preschool-age children.
The Preschool ADHD Treatment
Study (PATS) (2006) was designed to answer this call for further study. A small
handful of previous studies had produced conflicting results on MPH in preschool-age
children, with two identifying no difference in response to placebo and MPH25-26
and one indicating increased adverse events in younger children taking MPH as
opposed to older children on MPH.27 These studies were subject to
methodological differences, particularly in relation to inclusion/exclusion
criteria. The PATS was a large, multi-site trial with rigorous criteria for
inclusion and exclusion. Prior to admittance to the study, prospective subjects
underwent extensive assessment, and all cases required a consensus agreement of
acceptability from a cross-site panel of clinicians prior to admittance.
The study found significant
evidence for the efficacy of MPH in preschool-age children when administered
2.5, 5, and 7.5 mg TID. No significant improvement was found for children receiving
1.25 mg TID. The optimal dose for the preschoolers was 14.2±8.1 mg/day. Significantly higher doses were
required for maintenance of response during the 10-month treatment period.
Despite the
reduction of ADHD symptoms in the PATS subjects taking MPH, effect sizes were
significantly lower than those recorded in prior studies of older children. The
authors suggest this could be due to age-specific differences in treatment
response, differences in study design between PATS and prior large studies of
MPH response in older children, or a combination thereof.
Safety and Tolerability of MPH
The
5 most common adverse events (AEs) in the PATS were decreased appetite,
difficulty sleeping, repetitive behaviors, emotional outbursts, and
irritability. Parent-rated AEs for MPH that were significantly greater than
those for placebo were appetite decrease, trouble sleeping, and weight loss. No
significant differences in AEs were recorded between different dose sizes of
MPH. No cardiovascular AEs were observed.
 The
PATS uncovered notable differences between AEs in preschool-age children on MPH
and older children on MPH. Discontinuation rates were higher in PATS (11%) than
in the large, MTA Cooperative Study Group (1999) examination of MPH in
school-age children (<1%). Furthermore, preschool-age children demonstrated
a different profile of moderate to severe AEs than that found in school-age
children. The latter were subject to decreased appetite, delay of sleep onset,
headaches, and stomach aches.
The
PATS uncovered notable differences between AEs in preschool-age children on MPH
and older children on MPH. Discontinuation rates were higher in PATS (11%) than
in the large, MTA Cooperative Study Group (1999) examination of MPH in
school-age children (<1%). Furthermore, preschool-age children demonstrated
a different profile of moderate to severe AEs than that found in school-age
children. The latter were subject to decreased appetite, delay of sleep onset,
headaches, and stomach aches.
The MPH-related AEs in
preschool-age children with ADHD, although more aversive than in their older
counterparts, appeared, on the whole, manageable. The authors of the PATS
noted, however, that a much larger study (N>1,500) is required to meet
regulatory guidelines for establishing side-effect profile.
Evidence
also suggests28 that persistent treatment with a stimulant can
significantly lower the growth rate in young children; however, this
possibility needs to be balanced against the likely benefit of treatment on a
case-by-case basis.
The
related finding that preschool-age children require higher concentrations of
MPH in their blood to achieve the same behavioral effects as those seen in
school-age children is somewhat surprising.29 Medication absorption
and clearance is likely affected not just by weight, but by differences in
physiology (as relating to either structure or particular enzymes) between
younger and older children. Further analysis of these relationships is critical
to properly inform dosing. It seems evident that size and weight are not the
only salient factors.30
Psychosocial Treatment
The
MTA study of school-age children with ADHD found that, while medication
treatment as delivered in the study was highly effective, behavioral treatment
was equally effective to the medication treatment delivered in the community,
and combination therapy was most effective of all. However, these differences
disappeared at follow-up. The PATS did not examine behavioral treatments in
preschool-age children, but rather, parent training prior to initiation of
medication treatment. Prior work demonstrated that parent training produced
clinically significant symptom improvement in preschool-age children with ADHD
(as well as increasing ratings of maternal well-being).31
The
success of psychosocial treatment in older children, preliminary evidence for
the efficacy of behavioral treatments in preschool-age children, the
side-effect profile of stimulants in young children, and issues surrounding
parent resistance to medicating their children all warrant further study of
psychosocial intervention and combination therapy in young children with ADHD.
While some parents turn to alternative treatments—eg, natural supplements—there
is currently no evidence supporting their efficacy.
In summary, both medication and
behavioral treatments appear to alleviate the symptoms of ADHD. Most evidence
suggests that discontinuation of treatment leads to the reemergence of the
condition. ADHD is a chronic problem. At the present time, efforts are
continuing towards understanding the genetic underpinnings of ADHD. Early
identification and treatment of symptoms of ADHD preschool-age children may
contribute to more positive outcomes.
To take the free, online CME post-test, go to www.mssmtv.org/psychweekly
References
1. Lavigne JV, Gibbons RD, Christoffel KK, et al. Prevalence rates and correlates of psychiatric
disorders among preschool children. J
Am Acad Child Adolesc. 1996;32:204-214.
2. Campbell SB. Parent-referred problem three-year-olds: developmental changes in symptoms. J Child Psychol
Psychiatry.
1987;28:835-845.
3. DuPaul GJ, McGoey KE, Eckert TL, VanBrakle J. Preschool children with attention-deficit/hyperactivity
disorder: impairments in behavioral, social, and school functioning. J Am Acad Child Adolesc.2001;40:508-515.
4. Lahey BB, Pelham WE, Stein MA, et al. Validity of DSM-IV attention-deficit/hyperactivity
disorder for younger children. J
Am Acad Child Adolesc. 1998;37:695-702.
5. LaHoste GJ, Swanson JM, Wigal SB, et al. Dopamine D4 receptor gene polymorphism is associated
with attention deficit hyperactivity disorder. Mol Psych. 1996;1:121-124.
6. Lahey BB, Pelham WE, Loney J, et al. Three-year predictive validity of DSM-IV attention
deficit hyperactivity disorder in children diagnosed at 4Y6 years of age. Am J Psychiatry. 2004;161:2014-2020.
7. Pierce EW, Ewing LJ, Campbell SB. Diagnostic status and symptomatic behavior of hard-to-manage
preschool children in middle childhood and early adolescence. J Clin Child Psychol. 1999;28:44-57.
8. Wilens TE, Biederman J, Brown S, Monuteaux M, Prince J, Spencer TJ. Patterns of psychopathology
and dysfunction in clinically referred preschoolers. J Dev Behav Pediatr. 2002;23:S31-S36.
9. Medco Health Solutions. 2004 Drug Trend Report. www.medcohealth.com. Accessed May 17,
2004.
10. Zito JM, Safer DJ, dosReis S, Gardner JF, Boles M, Lynch F. Trends in the prescribing of psychotropic medications
to preschoolers. JAMA.
2000;283:1025-1030.
11. Manidiaki K, Sonuga-Barke E, Kakouros E, Karaba R. Parental beliefs about the nature of ADHD behaviours and their
relationship to referral intentions in preschool children. Child Health Care Dev. 2007;33:188.
12. Consensus Development Panel. Defined Diets and Childhood Hyperactivity. National Institutes of Health Consensus Development
Conference Summary, Volume 4, Number 3, 1982.
13. Biederman J, Faraone SV, Keenan K, Knee D, Tsuang MF. Family-genetic and psychosocial risk factors in DSM-III attention
deficit disorder. J Am Acad Child Adolesc Psychiatry. 1990;29:526-533.
14. Faraone SV, Biederman J. Neurobiology of attention-deficit hyperactivity disorder. Bio Psych. 1998;44;951-958.
15. Faraone SV, Perlis RH, Doyle AE, et al. Molecular genetics of attention-deficit/hyperactivity disorder. Bio Psych,.
2005;57:1313-1323.
16. Kennedy JL. Dopamine D4 receptor gene polymorphism is associated with attention deficit
hyperactivity disorder. Mol
Psych. 2004;1:121-124.
17. Lowe N, Kirley A, Hawi Z, et al. Joint analysis of the DRD5 marker concludes association with attention-deficit/hyperactivity
attention-deficit/hyperactivity disorder confined to the predominantly inattentive and combined subtypes. Am J Hum
Genet. 2004;74:348-356.
18. El-Faddagh, M., Laucht, M., Maras, A., et al. Association of dopamine D4 receptor (DRD4) gene with attention-deficit/hyperactivity
disorder (ADHD) in a high-risk community sample: a longitudinal study from birth to 11 years of age. J Neur Trans.
2004;111: 883-889.
19. Swanson JM, Kraemer HC, Hinshaw SP, et al. Clinical relevance of the primary findings of the MTA: success rates based
on severity of ADHD and ODD symptoms at the end of treatment. J Am Acad Child Adolesc. 2001:40;168-179.
20. Thapar A, Langley K, Fowler T, et al. Catechol o-methyltransferase gene variant and birth weight predict early-onset
antisocial behavior in children with attention-deficit/hyperactivity disorder. Archives of General Psychiatry.
2005;62:1275-1278.
21. Thapar A, Langley K, O’Donovan M, et al. Refining the attention deficit hyperactivity
disorder phenotype for molecular genetic studies. Mol Psych. 2006;11:714 –720.
22. MTA Cooperative Group. A 14-month randomized clinical trial of treatment strategies for attention deficit hyperactivity
disorder. Arch Journ Psych. 1999;56:1073-1086.
23. Wender PH. ADHD: Attention-Deficit Hyperactivity Disorder in Children and Adults. Oxford University Press.
2002;p. 9.
24. Geller B, Williams M, Zimerman B, Frazier J, Beringer L, Warner KL. Prepubertal and early adolescent bipolarity differentiate
from ADHD by manic symptoms, grandiose delusions, ultra-rapid or ultradian cycling. J Affect Disord. 1998;51:81-91.
25. Barkley RA, The effects of methylphenidate on the interactions of preschool ADHD children with their mothers. J
Am Acad Child Adolesc. 1998;27:336-341.
26. Cohen NJ , Evaluation of the relative effectiveness of methylphenidate and cognitive behavior modification in the
treatment of kindergarten-aged hyperactive children. J Abnormal Child Psychol. 1981;9:43-54.
27. Handen BL, Feldman HM, Lurier A, Murray PJ. Efficacy of methylphenidate among preschool children with developmental
disabilities and ADHD. J Am Acad Child Adolesc. 1999;38:805-812.
28. Swanson J, Greenhill L, Wigal T, et al. Stimulant-related reductions of growth rates in the PATS. J Am Acad Child
Adolesc.
2006;45:1304-1313.
29. Wigal S, Gupta S, Greenhill L, et al. Pharmacokinetics of Methylphenidate in Preschoolers With Attention-Deficit/Hyperactivity
Disorder. J Child Adolesc Psychopharm. In press.
30. Greenhill L, Kollins S, Abikoff H, et al. Rationale, Design, and Methods of the Preschool ADHD Treatment Study (PATS). J
Am Acad Child Adolesc. 2006;45:11.
31. Sonuga-Barke EJ, Daley D, Thompson M, Laver-Bradbury C, Weeks A. Parent-based therapies for preschool attention-deficit/hyperactivity
disorder: a randomized, controlled trial with a community sample. J Am Acad Child Adolesc. 2001;40:402-408.
32. Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition. Washington, DC; American Psychiatric
Association:1994.
33. McGough JJ. Attention-deficit/hyperactivity disorder pharmacogenomics. Bio Psych. 2005;57:1367-1373.
34. Kollins S, Greenhill L, Swanson J, et al. Rationale, design, and methods of the Preschool ADHD Treatment Study (PATS). The
J Am Acad Child Adolesc. 2006;45:1275-1283.
To take the free, online CME post-test, go to www.mssmtv.org/psychweekly