Click here to go to the CME post-test
Print Friendly
Special Considerations in Diagnosing and Treating ADHD
Part 2: Children and Adolescents
Sharon Wigal, PhD
Clinical Professor of Pediatrics, University of California, Irvine
Timothy Wigal, PhD
Associate Clinical Professor of Pediatrics, University
of California, Irvine
This is the second in a 3-part Psychiatry Weekly CME series on special considerations in diagnosing and treating ADHD. Part
1 focused on the preschool-age population, and part
3 will focus on the adult population.
Accreditation
Statement

This
activity has been planned and implemented in accordance with the Essentials and Standards of the Accreditation Council
for Continuing Medical Education (ACCME) through the joint sponsorship of the Mount
Sinai School of Medicine and MBL Communications, Inc. The Mount Sinai School of
Medicine is accredited by the ACCME to provide continuing medical education for physicians.
Credit
Designation
The
Mount Sinai School of Medicine designates this educational activity for a
maximum of 1 AMA PRA Category 1 Credit(s)TM. Physicians
should only claim credit commensurate with the extent of their participation in
the activity.
Faculty
Disclosure Policy Statement
It is the policy of the Mount Sinai School of Medicine to
ensure objectivity, balance, independence, transparency, and scientific rigor
in all CME-sponsored educational activities. All faculty participating in the
planning or implementation of a sponsored activity are expected to disclose to
the audience any relevant financial relationships and to assist in resolving
any conflict of interest that may arise from the relationship. Presenters must
also make a meaningful disclosure to the audience of their discussions of unlabeled
or unapproved drugs or devices.
This
activity has been peer reviewed and approved by Eric Hollander, MD, Professor
of Psychiatry and Chair at Mount Sinai School of Medicine. Review Date: May 9, 2007
Statement of Need
ADHD is the most common
childhood psychiatric disorder, and children with the disorder are subject to
long-term social and academic impairment. The cost to society has been estimated
at over 30 billion dollars per year. Diagnosis of ADHD in school-age children
and adolescents requires the presence of symptoms in two or more different
environments and generally involves symptom assessments from both parents and
teachers. The diagnosis is further complicated by the high frequency of
comorbid psychiatric disorders in this patient population. ADHD is strongly
genetic, but no specific genes have yet been implicated in the disorder.
Medication,
psychosocial therapy, and combined treatment have all been shown effective for
reducing symptoms, but ADHD does not fully resolve, either on its own or with
treatment. School-age children and adolescents with ADHD need effective,
long-term symptom management. Non-amphetamine medications are being explored,
and some have demonstrated success, but amphetamines are still the most
effective medication in reducing ADHD symptoms. Treatment noncompliance is
high, particularly in older children and adolescents—new methods of drug
delivery are being explored to address this issue.
An important educational need exists to
improve identification of ADHD by both psychiatrists and general
practitioners. Clinicians must also stay abreast of the evidence on efficacy,
adverse events, and compliance for pharmacotherapeutic, behavioral, and combined
treatments.
Learning Objectives
- Describe the impact of ADHD on children and adolescents and the difficulties
inherent in diagnosing this patient population.
- Assess the evidence on treatment efficacy, safety, and compliance in
children and adolescents with ADHD.
- Explain the current information on the etiology and likely course of ADHD in
children and adolescents with ADHD, and understand how this impacts diagnosis
and treatment.
Target Audience
This activity will
benefit psychiatrists, hospital staff physicians, and office-based “attending”
physicians from the community.
Funding/Support
This activity is supported by an educational
grant from Shire.
Faculty Disclosures
Sharon
Wigal, PhD, has disclosed that she has received research support from
Cephalon, Eli Lilly, McNeil, New Rivers, NIH, and Shire; has served as an
advisor or consultant to Cephalon, McNeil, New Rivers, Novartis, Shire, and
UCB; and has served on the speaker’s bureau for McNeil, Shire, and UCB.
Timothy Wigal, PhD, has disclosed that
he has received research support from Cephalon, Eli Lilly, McNeil, New Rivers,
NIH, Novartis, and Shire; has served as a consultant or advisor to McNeil,
Novartis, and Shire; and has served on the speaker’s bureau of McNeil and Shire.
Peer Reviewers
Eric Hollander, MD, reports no
affiliation with or financial interest in any organization that may pose a
conflict of interest
Daniel Stewart, MD, PhD, reports no
affiliation with or financial interest in any organization that may pose a conflict
of interest.
To Receive Credit for this Activity
Read
this poster, reflect on the information presented, and then complete the CME
quiz found in the accompanying brochure or online (www.mssmtv.org/psychweekly).
To obtain credit you should score 70% or better. The estimated time to complete
this activity is 1 hour.
Release Date: June 6, 2007
Termination Date: June 6, 2009
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is the most common childhood psychiatric disorder.1 Children
who suffer from the disorder are subject to significant short- and long-term academic deficiencies,2 social
impairment,3 and the overall annual societal cost of the disorder has been estimated at 36-52.4 billion dollars
($12,005-$17,548 per child per year, 5% prevalence).4 Contrary to previous belief, the disorder does not resolve
with puberty for the majority of children.5-6 Diagnosis is particularly difficult due in large part to the pronounced
comorbidity of psychiatric disorders in this patient population,7 which can result in both over- and under-diagnosis.8-10 Difficulties
are compounded by the large role of primary care practitioners—who may not be as familiar with the disorder as psychiatrists—in
both diagnosis and treatment.11 Clearly, ADHD presents a critical challenge to public health in America. Identifying
and aggressively treating ADHD in children and adolescents is essential to effective long-term management of the disorder.
Prevalence
Prevalence
estimates of ADHD in school-aged children (4-17 years) are widely disparate.
One extensive review found estimates ranging from 2%-18% of American children
in community samples.12 The National Institute of Mental Health
(NIMH) estimates the prevalence of ADHD in children at 3%-5%13.
According to a Center for Disease Control analysis of the 2003 National Survey
of Children’s Health (which surveyed parents or guardians of over 100,000 children)
approximately 4.4 million American children and adolescents (7.8% of those aged
4-17) had a history of ADHD diagnosis. In addition, approximately 2.4 million
children (4.3% of those aged 4-17) were found to both have a diagnosis of ADHD
and received medication to treat ADHD.14 Males were 2.5 times more
likely to have been diagnosed than females, and the highest prevalence was
among 16-year-old males (14.9%) and among 11-year-old females (6.1%).
Prevalence of diagnosis was significantly higher for children and adolescents
with insurance and primarily from English-speaking families.
Impact
ADHD in children and adolescents is significantly
associated with disability.
This patient population is prone to below average
academic performance, increased risk of substance abuse, emotional problems,
difficulty with peer relationships, and legal troubles.2,15-17
Teenagers with ADHD who are of driving age are at increased risks for
accidents.18 Parents who have adolescents with ADHD are also
severely impacted; they are subject to chronic stress, and this can have a
negative effect on both the parents and other family members.19
Comorbidities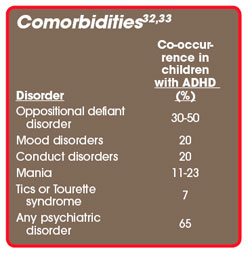
Children with ADHD are at significantly increased risk
for other psychiatric disorders, including mood, anxiety, and conduct disorders,
and in adolescents, substance abuse disorders.20 Children with ADHD
are also extremely prone to learning disabilities, with estimates of prevalence
ranging from 10% to 92%.21 Comorbid disorders can both worsen the
course of ADHD and impact treatment. For example, anxiety in this patient
population is associated with increased psychiatric treatment and impaired
psychosocial functioning.22
Oppositional Defiant Disorder
and Conduct Disorder
Oppositional Defiant Disorder (ODD) and Conduct Disorder
(CD) co-present with ADHD in 30% to 50% of children23 and are of
particular note in that they significantly impact the course of ADHD in
children and are linked to other comorbidities in this patient population. ODD
entails pronounced hostile and defiant behavior, while CD is considered more
severe, and involves habitual rule breaking defined by aggression, destruction,
and lying. CD nearly always follows ODD, however, it has recently been found
that ODD is a poor predictor of later CD onset. Further, ODD + CD is a strong
predictor of substance abuse, while ODD alone is not. There is evidence that,
despite its correlation with more serious clinical course of ADHD, CD does not
significantly alter treatment course in children with ADHD.24-26
Mood Disorders
Lifetime rates of comorbid depression in children with
ADHD range from 29-45%, and comorbid depression predicts impaired psychosocial
and interpersonal functioning, as well as higher hospitalization rates. Mania
is present in 11-23% of children with ADHD and correlates to impaired psychosocial
functioning, psychiatric hospitalization, and additional psychopathology.27
There have also been indications that comorbid bipolar disorder is correlated
with an increased risk of completed suicide attempts.28 Mania and
depression can both complicate an ADHD diagnosis, due to shared developmental
features, but adolescent mania can be more differentiable from ADHD, as the
symptoms of the latter are likely to have preceded the symptoms of the former
by a number of years. There is evidence that mood disorders and ADHD share similar
genetic risk factors.29
Comoribidity and Treatment
Response
The
response to medication treatment is variable, and many children are not
excellent responders30 despite careful titration and management.
Treatment may be more successful depending on the presence of co-morbid
conditions. In general, it has been suggested that a less favorable response to
stimulant treatment for patients with ADHD is correlated with an increase in
the number of co-morbid disorders. For example,
the Multimodal Treatment Study of Children with ADHD (MTA) study, a large,
randomized controlled clinical trial in children with ADHD, noted that
treatment outcome was moderated by both anxiety and depressive symptoms.31
This study is of note because it is free of a referral bias sometimes associated with other studies.
Diagnosis
The Diagnostic and Statistical Manual of Mental
Disorders, Fourth Edition (DSM-IV) criteria for ADHD were originally
based on presentation in school-aged children, so diagnosing school-age
children with ADHD is more straightforward than diagnosing their younger and
older counterparts. The criteria require either 6 or more symptoms of
inattention or 6 or more symptoms of hyperactivity-impulsivity, persisting for
at least six months, inconsistent with developmental level, and producing
significant impairment. There must also be evidence that some symptoms causing
impairment were present before the age of 7, impairment must be present in at
least two settings, and symptoms cannot be better accounted for by another
mental disorder.34 ADHD occurs as one of three subtypes—combined,
inattentive, or hyperactive-impulsive—depending on the relative representation
of the symptom domains.
Generally, the two settings analyzed for presentation of
symptoms are home and school.
Parents
or guardians are predominately responsible for providing information on a young
child’s symptoms at home, but they can either over- or under-represent the
frequency and severity of symptoms. Due to the high heritability of ADHD, it is
very likely that a parent of a child with ADHD will also have symptoms of the
disorder, which can interfere with the parent’s role in the diagnosis. Parents’
perceptions can also be impaired by the lack of a good comparator group. Unlike
a child’s teacher, parents may not have witnessed enough behavior from other
children to accurately compare their own child’s behavior and attention
relative to age-matched peers. There is some evidence that over-reliance on
parental reports of symptoms leads to overdiagnosis, while clinician assessment
of symptoms in their office and self-report from young children result in
underdiagnosis.38
One study39 found a 74% concordance between
parent and teacher assessment of symptoms in younger children with ADHD, and
this concordance rate only falls as children grow into adolescence. While
children in elementary school primarily will spend the entire school day with
one teacher, children in secondary education will have up to 7 separate
teachers a day. Not surprisingly, inter-rater reliability tends to be low among
secondary school teachers when assessing their students.40 Older
children and adolescents are also likely to spend a great deal less time at
home, making it more difficult for the parents to assess their symptoms. There
is also evidence that adolescents are as unlikely to accurately report their
own symptoms as are younger children.41
Collecting evidence of ADHD symptoms present before the
age of 7 in adolescents also presents difficulties as parent, teacher, and
self-report are all likely have difficulties with retrospective recall. A
review of school reports should always be included in all ADHD diagnosis in
children and adolescents, and have particular value as an aid in recall of past
problems.31 Diagnosing ADHD for all age groups is complicated by the
high prevalence of comorbid psychiatric disorders in this population. Children
and adolescents with opposition defiant disorder, bipolar disorder,42
and a variety of anxiety disorders can present quite similarly to ADHD.10
Therefore, a careful differential diagnosis is a necessary and crucial part of
the diagnostic process.
Clinicians diagnosing patients who may have ADHD should
make liberal use of rating scales, which aid not only in identifying symptoms of
ADHD, but, equally important, other psychiatric disorders that might confound
diagnosis. Scales can be roughly broken down into “narrow”—those that focus
specifically on ADHD, and “broad”—those that measure a broader range of
behaviors. Patient self-report scales can augment parent and teacher report
scales, but the clinician must remember that adolescents are extremely likely
to under-represent their symptoms.
There is some debate over the relative prevalence of
ADHD in boys and girls. Until recently, 6 boys were diagnosed for every girl
who was diagnosed with ADHD. Now, the ratio is closer to 3:1. Some suggest that
ADHD may still be underdiagnosed in girls, perhaps due to parent and teacher
preconceptions about gender disparity in ADHD.49 Studies on gender
differences in presentation of ADHD are few and conflicting. Some have found no
significant difference in symptomatology, comorbidity, and neuropsychological
function,50,51 while others suggest that girls with ADHD demonstrate
lower levels of activity and aggression.52,53
Treatment
According to the results of the collaborative, multisite
NIMH-funded, Multimodal Treatment Study of Children With Attention-Deficit/Hyperactivity
Disorder (MTA)—with 579 probands the largest randomized clinical trial of
treatment for ADHD ever attempted—behavioral treatment is effective in children
with ADHD, but both medication treatment and combined behavioral and medication
treatment demonstrate even greater efficacy.54 Of note, treatment
regimens in the MTA study—although constrained to one of four treatment arms:
medication, behavioral, combined treatment, or community-treatment/assessment
and referral, did allow for some individual flexibility in terms of the
intensity of the treatment that was administered. In other words, each
treatment arm was developed as a “management strategy,” allowing for a certain
degree of flexibility in responding to the individual needs of the patients who
may have needed a different dose schedule or “extra” counseling.
Recently,
the field of ADHD treatment has experienced some excitement regarding atomoxetine, a norepinephrine re-uptake inhibitor
and the first FDA-approved non-stimulant medication for ADHD. Atomoxetine does not
carry the same potential for abuse as amphetamines do, and is less likely to
lead to some of the same types of side effects (e.g., insomnia) that can
sometimes prevent effective treatment. However, the precise mechanism of action of
atomoxetine in ADHD has remained elusive and stimulant treatment appears to be significantly more effective in
reducing symptom severity. In fact, the overall side effect profile is comparable between the two drugs.55
A number of alternative treatments for ADHD have also
been explored. According to one extensive review, enzyme-potentiated
desensitization, relaxation/EMG biofeedback, and deleading (a process of
supposedly removing lead from the body) have demonstrated some efficacy in
controlled trials; iron supplementation, magnesium supplementation, Chinese
herbals, EEG biofeedback, massage, meditation, mirror feedback,
channel-specific perceptual training, and vestibular stimulation have shown
some promise in prospective pilot studies. Oligoantigenic (few-foods) diets
appear somewhat effective for children, but do not appear to work for adults.
There are also a number of other alternative treatments with some promise, but
evidence of improved outcome is still very sparse.56
Treatment compliance is a particular concern in treating
ADHD, but recent advances in drug delivery show some promise in reducing
noncompliance in this patient population. Once-a-day amphetamine treatments
have been available for ADHD patients since 2000, and recently, researchers
have been exploring other alternative methods of delivery for methylphenidate.
Of particular note are the osmotic-release delivery system and the transdermal
delivery system. Osmotic release provides consistent drug delivery throughout
the day. The transdermal delivery system or patch has the advantage of ease of
administration while maintaining efficacy for patients who have difficultly
swallowing or tolerating oral treatments.57
To take the free, online CME post-test, go to www.mssmtv.org/psychweekly
References
1.
Olfson M. Diagnosing mental disorders in office-based pediatric practice. J Dev
Behav Pediatr. 1992;13:363-365.
2.
Frazier T, Youngstrom E, Glutting J, Watkins M. ADHD and Achievement:
Meta-Analysis of the Child, Adolescent, and Adult Literature and a Concomitant
Study With College Students. Journal of Learning Disabilities. 2007;40:49-65.
3.
Bagwell C, Molina B, Pelham W, Hoza B. Attention deficit hyperactivity disorder
and problems in peer relations: predictions from childhood to adolescence. J Am
Acad Child Adolesc Psychiatry. 2001;40:1285-1292.
4.
Pelham W, Foster M, Robb J. The Economic Impact of Attention-Deficit/Hyperactivity
Disorder in Children and Adolescents. Ambulatory Pediatrics. 2007;7:121-131.
5.
Biederman J, Farone S, Milberger S, et al. A prospective 4-year follow-up study
of attention-deficit/hyperactivity and related disorders. Arch Gen Psychiatry.
1996;53:437-446.
6.
Ingram S, Hechtman L, Morgenstern G. Outcome issues in ADHD: adolescent and
adult long-term outcome. Ment Retard Dev Disabil Res Rev. 1999;5:243-250.
7.
Biederman J, Newcorn JH, Sprich S. Comorbidity of attention-deficit
hyperactivity disorder with conduct, depressive, anxiety and other disorders.
Am J Psychiatry. 1991;148:251-256.
8.
Abikoff H, Courtney M, Pelham WE, Koplewicz HS. Teachers’ ratings of disruptive
behaviors: the influence of halo effects. J Abnorm Child Psychol. 1993;21:519-533.
9.
Schachar R, Sandber S, Rutter M. Agreement between teachers’ ratings and
observations of hyperactivity, inattentiveness and defiance. J Abnorm Child
Psychol. 1986;14:331-345.
10.
Pliszka SR. Effect of anxiety on cognition, behavior and stimulant response in
ADHD. J Am Acad Child Adolesc Psychiatry. 1989;28:882-887.
11.
Rappley MD, Gardiner JC, Jetton JR, Houang RT. The use of methylphenidate in
Michigan. Arch Pediatr Adolesc Med. 1995;149:675-679.
12.
Rowland AS, Lesesne CA, Abramowitz AJ. The epidemiology of
attention-deficit/hyperactivity disorder (ADHD): a public health view. Mental
Retardation Developmental Disability Research Review 2002;8:162--70.
13.
NIMH. Attention Deficit Hyperactivity Disorder. 2006.
http://www.nimh.nih.gov/publicat/adhd.cfm#intro. Accessed April 19, 2007.
14.
Mental Health in the United States: Prevalence of Diagnosis and Medication
Treatment for Attention-Deficit/Hyperactivity Disorder --- United States, 2003.
MMWR. September 2, 2005 / 54(34);842-847.
15.
Wilens T. Alcohol and other drug use and attention deficit hyperactivity
disorder. Alcohol Health Res World. 1998;22:127-130.
16.
Gittelman R, Mannuzza S, Shenker R, Bonagura N. Hyperactive boys almost group
up: I. Psychiatric status. Arch Gen Psychiatry. 1985;42:937-947.
17.
Hechtman L, Weiss G. Controlled prospective fifteen year follow-up of
hyperactives as adults: non-medical drug and alcohol use and anti-social
behaviour. Can J Psychiatry. 1986;31:557-567.
18.
Barkley R. Driving Impairments in teens and adults with
attention-deficit/hyperactivity disorder. Psychiatr Clin North Am.
2004;27:233-260.
19.
Johnston C, Mash E. Families of children with attention deficit hyperactivity
disorder: review and recommendations for future research. Clin Child Family
Psychol. 2001;4:183-207.
20.
Biederman J, Wilens T, Mick E, et al. Does attention-deficit hyperactivity
disorder impact the developmental course of drug and alcohol abuse and dependence?
Boil Psychiatry. 1998;36:37-43.
21.
Silver LB. The relationship between learning disabilities, hperactivty,
distractibility, and behavioral problems. J Am Acad Child Psychiatry.
1981;20:385-397.
22.
Biederman J, Faraone SV, Mick E, et al. Attention deficit hyperactivity
disorder and juvenile mania: an overlooked comorbidity? J Am Acad Child Adolesc
Psychiatry. 1996;35:997-1008.
23.
Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit
hyperactivity disorder with conduct, depressive, anxiety, and other disorders.
Am J Psychiatry. 1991;148:564-577.
24.
Biederman J, Faraone SV, Milberger S, et al. Is childhood oppositional defiant
disorder a precursor to adolescent conduct disorder? Findings from a four-year
follow-up study of children with ADHD. J Am Acad Child Adolesc Psychiatry.
1996;35:1193-1204.
25.
Biederman J, Newcorn J, Sprich S. Comorbidity of Attention Deficit
Hyperactivity Disorder With Conduct, Depressive, Anxiety, and Other Disorders.
Am j Psychiatry. 1991;148:564-577.
26.
Klorman R, Brumaghim JT, Salzman LF, et al. Effects of methylphenidate on
attention-deficit hyperactivity disorder with and without
aggressive/noncompliant features. J Abnorm Psychol. 1988;97:413-422.
27.
Biederman J, Faraone SV, Keenan K, et al. Further evidence for family-genetic
risk factors in attention deficit hyperactivity disorder. Patterns of
comorbidity in probands and relatives in psychiatrically and pediatrically
referred samples. Arch Gen Psychiatry. 1992;49:728-738.
28.
Brent DA, Perper JA, Goldstein CE, et al. Risk factors for adolescent suicide:
a comparison of adolescent suicide victims with suicidal inpatients. Arch Gen
Psychiatry. 1988;45:581-588.
29.
Biederman J, Faraone S, Keenan K, et al. Family genetic and psychosocial risk
factors in attention deficit disorder. Biol Psychiatry. 1989;25:145A.
30.
Swansom JM, Kraemer HC, Hinshaw SP, et al. Clinical relevance of the primary
findings of the MTA: success rates based on severity of ADHD and ODD symptoms
at the end of treatment. J Am Acad Child Adolesc Psychiatry. 2001;40:168-179.
31.
The MTA Cooperative Group. A 14-month randomized clinical trial of treatment
strategies for attention-deficit/hyperactivity disorder. Multimodal Treatment
Study of Children with ADHD. Arch Gen Psychiatry. 1999;56:1073-1086.
32.
Spencer J, Biederman J, Mick E. Attention-Deficit/Hyperactivity Disorder:
Diagnosis, Lifespan, Comorbidities, and Neurobiology. Ambulatory Pediatrics.
2007;7:73-81.
33.
Goldman S, Genel M, Bezman R, Slanetz P. Diagnosis and Treatment of
Attention-Deficit/Hyperactivity Disorder in Children and Adolescents. JAMA.
1998;279:1100-1107.
34.
Diagnostic and Statistical Manual of Mental Disorders, Fourth Edition.
Washington, DC; American Psychiatric Association:1994.
35.
Morgan A, Hynd G, Riccio C, Hall J. Validity of DSM-IV ADHD predominately
inattentive and combined types: relationship to previous DSM diagnoses/subtype
differences. J Am Acad Child Adolsec Psychiatry. 1996;35:325-333.
36.
Paternite C, Loney J, Roberts M. External validation of oppositional disorder
and attention deficit disorder with hyperactivity. J Abnorm Child Psychol.
1995;23:453-471.
37.
Wolraich M, Hannah J, Pinnock T, et al. Comparison of diagnostic criteria for
attention-deficit hyperacitivty disorder in a country-wide sample. J Am Acad
Child Adolesc Psychiatry. 1996;35:319-324.
38.
Sleator E, Ullman R. Can the physician diagnose hyperactivity in the office?
Pediatrics. 1981;67:13-17.
39.
Mitsis E, McKay K, Schulz K, et al. Parent-teacher concordance for DSM-IV
attention-deficit/hyperactivity disorder in a clinic-referred sample. Child
Adolesc Psychiatry. 2000;39:308-313.
40.
Molina B, Pelham W, Blumenthal J, Galiszewski E. Agreement among teachers’
behavior ratings of adolescents with a childhood history of
attention-deficit/hyperactivity disorder. J Clin Child Psychol.
1998;27:330-339.
41.
Kramer T, Phillips S, hargis M, et al. Disagreement between parent and
adolescent reports of functional impairment. J Child Psychol Psychiatry.
2004;45:248-259.
42.
Geller B, Williams M, Zimerman B, Frazier J, Beringer L, Warner K. Prepubertal
and early adolescent bipolarity differentiate from ADHD by manic symptoms,
grandiose delusions, ultra-rapid or ultradian cycling. Journal of Affective
Disorders. 1998;51:81-91.
43.
Kiddie-Sads-Present and Lifetime Version (K-SADS-PL).
http://www.wpic.pitt.edu/ksads/default.htm. Accessed April 19, 2007.
44.
Achenbach T, Edelbrock L. Manual for the Child Behavior Checklist 4-18 and 1991
Profile. Burlington, VT: University of Vermont;1991.
45.
Reynolds C, Kamphouse R. BASC: Behavior Assessment System for Children Manual.
Circle Pines, MN: American guidance Service; 1992.
46.
Brown TE. Brown ADD Scales for Children and Adolescents. San Antonio, TX:
Psychological Corp; 2001.
47.
Swanson, Nolan and Pelham (SNAP) Questionnaire (Swanson et al, 1983).
48.
Shaffer D, Fisher P, Dulcan M, et al. The second version of the NIMH Diagnostic
Interview Schedule for Children (DISC-2). J Am Acad Child Adolesc Psychiatry.
1996;35:865-877.
49.
Quinn P, Wigal S. Perceptions of girls and ADHD: results from a national
survey. MedGenMed. 2004;6:2.
50.
Sharp WS, Walter J, Marsh W, Ritchie G, Hamburger S, Castellanos F. ADHD in
girls: clinical comparability of a research sample. J Am Acad Child Adolesc
Psychiatry. 1999;38:40-47.
51.
Biederman J, Faraone S, Milberger S, et al. Clinical correlates of ADHD in
females: findings from a large group of girls ascertained from pediatric and
psychiatric referral sources. J Am Acad Child Adolesc Psychiatry.
1999;38:966-975.
52.
Carlson C, Tamm L, Gaub M. Gender differences in children with ADHD, ODD and
co-occurring ADHD/ODD identified in a school population. J Am Acad Child
Adolesc Psychiatry. 1997;36:1706-1714.
53.
Gaub M, Carlson C. Gender differences in ADHD: a meta-analysis and critical
review. J Am Acad Child Adolesc Psychiatry. 1997;36:1036-1045.
54.
The MTA Cooperative Group. A 14-Month Randomized Clinical Trial of Treatment
Strategies for Attention-Deficit/Hyperactivity Disorder. Arch Gen Psychiatry.
1999;56:1073-1086.
55.
Wigal S, McGough J, McCracken J, et al. A laboratory school comparison of mixed
amphetamine salts extended release (Adderall XR) and atomoxetine (Strattera) in
school-aged children with attention deficit/hyperactivity disorder. J Atten
Disord. 2005;9:275:289.
56.
Arnold L. Alternative treatments for adults with attention-deficit
hyperactivity disorder (ADHD). Ann N Y Acad Sci. 2001;931:310-341.
57.
Wigal S, Wigal T, Kollins S. Advances in Methylphenidate Drug Delivery Systems
for ADHD Therapy. Advances in ADHD. 2006;1:4-7.
To take the free, online CME post-test, go to www.mssmtv.org/psychweekly