Print Friendly
Calming the Storm: Psychodynamic Treatment of Panic Disorder
Fredric N. Busch, MD
Dr. Busch is a clinical associate professor of psychiatry at the Weill Cornell
Medical College in New York City.
Disclosure: Dr. Busch reports no affiliation with
or financial interest in any organization that may pose a conflict of interest.
Please
direct all correspondence to: Fredric N. Busch, MD, Clinical Associate Professor
of Psychiatry, Department of Psychiatry, Cornell University, 10 East 78th St,
Apt. 5A, New York, NY 10021; Tel: 212-734-0257; Fax: 212-734-0257; E-mail: [email protected].
Abstract
This article describes the limitations of current treatments for panic disorder.
Despite demonstrations of effectiveness of cognitive-behavioral and psychopharmacologic
treatments, many patients fail to respond to these interventions or have persistence
or recurrence of symptoms. Given the high costs and morbidity of panic disorder,
there is a need to continue to explore treatment options. Psychoanalytic approaches
are commonly used for panic disorder but have undergone little systematic study.
This article describes the psychoanalytic concepts involved in understanding panic
disorder, and proposes a manualized psychodynamic psychotherapy for panic disorder
called panic-focused psychodynamic psychotherapy. A case example is used to demonstrate
some aspects of conducting treatment with this approach. This article also reviews
the limited systematic research on psychodynamic treatment of panic.
INTRODUCTION
Both
pharmacologic1-3 and cognitive-behavioral treatments4-6
of panic disorder have been found to be effective in the short-term treatment
of panic disorder. However, many patients fail to respond to or are unable to
tolerate these treatments.4-8 Relapse is frequent if medication is
discontinued before a prolonged maintenance phase.9-12 In addition,
questions remain about the long-term effectiveness of these interventions.4,13
In studies of routine care, patients frequently demonstrate persistent symptoms
and problems functioning.14 Finally, these treatments may not be as
effective in treating impairments associated with panic disorder, such as
occupational dysfunction, relationship difficulties, and diminished quality of
life.15,16 Given the high morbidity and health costs of this
disorder,17-20 it is important to develop the most effective
treatments for panic disorder and related impairments.
A
commonly used but not well-studied treatment for panic disorder is
psychodynamic psychotherapy. The potential value of this treatment is based on
the notion that panic patients have a psychological vulnerability to the
disorder associated with “personality disturbances, relationship problems,
difficulties tolerating and defining inner emotional experiences, and unconscious
conflicts about separation, anger and sexuality.”21 Psychodynamic
treatments focus more on these impairments than cognitive-behavioral and
psychopharmacologic treatments, potentially reducing vulnerability to panic
recurrence.21 The author of this article and colleagues developed a
psychodynamic formulation for panic disorder based on psychoanalytic theory,
systematic psychological assessments, and clinical observations to guide
treatment interventions.21-23 This article describes psychoanalytic
concepts as they relate to panic disorder, followed by a psychodynamic
formulation that weaves together neurophysiologic and psychological
vulnerabilities to panic.
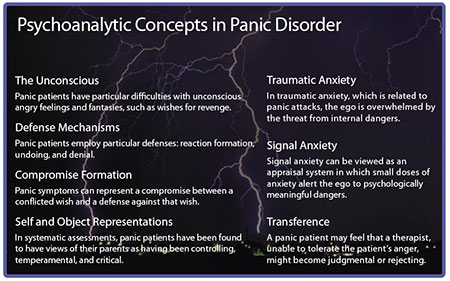
Psychoanalytic Concepts in Panic Disorder
The Unconscious
According
to psychoanalytic theory, symptoms are based at least in part on unconscious fantasies
and affects.24 For example, clinical and research observation
suggests that panic patients have particular difficulties with angry feelings
and fantasies, such as wishes for revenge.22,23,25 These wishes
represent a threat to important attachment figures, thus triggering anxiety.
Patients are often unaware of the intensity of these affects and the vengeful
fantasies that accompany them. Becoming aware of these aspects of mental life
and rendering them less threatening are important components of psychodynamic
psychotherapy.
Defense Mechanisms
Fantasies
and affects that are experienced as dangerous can be dealt with through the triggering
of defenses, that is, mental processes that disguise the fantasies or render
them unconscious.26 Clinical and research observations indicate that
panic patients employ particular defenses: reaction formation, undoing, and
denial.27 Reaction formation and undoing play a particular role for
panic patients in that they attempt to convert an angry affect into a more affiliative
one, diminishing the threat to an attachment figure. In reaction formation a
threatening feeling is replaced by its opposite; negative feelings of panic
patients are oftentimes replaced by concern and efforts to help others. In
undoing, a negative affect or fantasy is typically taken back in some way.
Denial represents a lack of recognition of the presence of a particular feeling
or fantasy, such as a patient reporting he was not angry even after someone had
done something hurtful to him. It is generally important to bring these
defenses to the patient’s attention as they maintain the patient’s avoidance of
exploring the frightening feelings and fantasies. For example, a patient who
follows the statement “I hate him” by “but I really love him” (an example of
undoing), is often trying to avoid the intensity of his angry feelings.
Compromise Formation
A
symptom can represent a compromise between a conflicted wish and a defense
against that wish.24 Teasing apart the components of this compromise
formation can help to understand the meaning of that symptom and the
unconscious factors that are triggering it. Thus, panic symptoms can include
the wish to be taken care of, a denial of anger through a focus on anxiety or
bodily symptoms, and an unconscious expression of anger in the coercive aspect
of pressuring others to help.
Self and Object Representations
Particular
self and object representations can trigger a susceptibility to certain
symptoms. In systematic assessments, panic patients have been found to have
views of their parents as having been controlling, temperamental, and critical.28,29
These expectations of the behaviors of others are internalized. In addition,
because of their predisposition to fearfulness, panic patients have a view of
others as essential to their safety and well-being. Recognizing these perceptions
of self and others can help panic patients understand the danger they
experience in communicating wishes to be taken care of as well as angry
feelings.
Traumatic and Signal Anxiety
Freud
distinguished between “traumatic” and “signal” anxiety.30 In
traumatic anxiety, which is related to panic attacks, the ego is overwhelmed by
the threat from internal dangers. Signal anxiety, on the other hand, can be
viewed as an appraisal system in which small doses of anxiety alert the ego to
psychologically meaningful dangers, such as potential disruptions in attachment
or the threat from vengeful feelings. Signal anxiety can trigger defenses that
act unconsciously to ward off potential dangers. In panic-focused psychodynamic
psychotherapy (PFPP), the therapist works with anxiety to help the patient
cognitively reappraise the degree of actual danger he is in.
Transference
In the
course of treatment, conflicts that the patient experiences as occurring with
others will often be mirrored in the relationship with the therapist. For
example, a panic patient may feel that a therapist, unable to tolerate the
patient’s anger, might become judgmental or rejecting. This phenomenon,
referred to as transference, can provide direct access to intrapsychic conflicts
and self-and-object representations that underlie panic symptoms. The safe
environment provided by a nonjudgmental and collaborative therapist aids in the
emergence of transference feelings and fantasies.
Psychodynamic Formulation for Panic Disorder
Busch
and colleagues21 and Shear and colleagues22 developed a
psychodynamic formulation for panic disorder based on neurophysiologic
predispositions, psychological findings, and psychoanalytic theory. The
formulation posits that certain individuals are susceptible to the onset of
panic disorder due to a predisposition to anxiety associated with a fearful
temperament described by Kagan and colleagues.31 Because of their
anxiety, children with this predisposition tend to develop a fearful dependency
on others, feeling that the parents must be present at all times to provide a
sense of safety. In addition, the dependency on others is a narcissistic
humiliation for these children, because feelings of safety often require the
caregiver’s presence. This fearful dependency can develop from a biochemical
vulnerability or from an early relationship in which the children experience
frightening threats or behavior by caregivers. In either case, parents are
perceived as “unreliable,” and prone to abandonment and rejection of the child.
In
response to perceived rejection or unavailability, and due to the narcissistic
injury of dependency, the child becomes angry at his caregivers. This anger is
experienced as a danger, as it could potentially damage the relationship with
the caretakers upon whom the child depends, increasing the threat of loss and
fearful dependency. Thus, a vicious cycle of fearful dependency and anger can
occur. The vicious cycle is triggered again in adulthood, when the individual
experiences or perceives a threat to important attachment figures. Signal
anxiety and defenses are triggered, such as undoing, reaction formation, and
denial, in an attempt to reduce the threat from anger and maintain attachments.
However, due to the degree of threat from these fantasies, as well as
immaturity of the signal anxiety mechanism, the ego is overwhelmed and panic
levels of anxiety result. Panic attacks further avert the experience of anger
and compel attention from others to attend to the patient’s distress.
Recent
developments in psychoanalytic theory elucidate another component of the
process of panic onset and persistence. Mentalization describes the ability to
understand self and others with regard to motives, desires, and feelings.32
Panic patients may have either a diminished capacity for mentalization in
general or specific disruptions in this ability caused by conflicts regarding
dependency and angry feelings and fantasies. This lack of access to feelings and
fantasies can be viewed as unconscious efforts to “not know” about conflicts in
order to avoid the threat to attachment.33 Greater introspective
access and mentalization about emotional states of the self and others helps to
relieve these dangers. This can allow panic patients to develop voluntary
“top-down” cognitive control over emotional reactions by selectively inhibiting
and modifying them.
Panic-Focused Psychodynamic Psychotherapy
Overview of PFPP
As
opposed to more traditional open-ended psychodynamic treatment and
psychoanalysis, PFPP focuses on panic symptoms and the dynamics associated with
panic disorder. Material in the sessions other than panic symptomatology is
ultimately related to the dynamics of panic. The treatment follows the overall
course of identifying the meanings of panic symptoms; calling attention to
defenses that inhibit awareness of frightening feelings, conflicts, and
fantasies; and, once made conscious, rendering these feelings less threatening
or less toxic. Psychoanalytic techniques of clarification, confrontation, and
interpretation are employed in this process.
Phase I
In
phase I, the therapist works to identify the specific content and meanings of
the panic episode. In addition, the patient and therapist examine the stressors
and feelings surrounding the onset and persistence of panic. The patient’s
developmental history is reviewed to delineate specific vulnerabilities that
may have led to panic onset, such as particular representations of parents,
traumatic experiences, and difficulty expressing and managing angry feelings.
The therapist’s nonjudgmental stance aids the patient in bringing forth
fantasies and feelings that may have been unconscious or difficult to tolerate,
such as vengeful wishes or abandonment fears. The information is used to
identify the presence of intrapsychic conflicts surrounding anger, separation,
and sexuality. The goal of this phase is reduction in panic symptoms.
Phase II
Phase
II seeks to address the dynamics that lead the patient to be vulnerable to
panic onset and persistence. As noted above, these typically include conflicts
surrounding anger recognition and management, separation, and fears of loss or
abandonment. These dynamics are addressed as they emerge in the patient’s
feelings and fantasies about relationships in their present and past and in the
transference relationship with the therapist. The meanings of symptoms and the
employment of defenses also continue to play a role in identifying the dynamic
constellations. Improved understanding of these conflicts helps patients to
prevent the development of the vicious cycle described in the formulation
above, reducing vulnerability to panic disorder recurrence.
Phase III
The
termination phase provides an opportunity to work with the patient’s conflicts
with anger and separation as they emerge in the context of ending treatment.
Patients can experience and articulate their feelings about loss directly with
the therapist. This increased awareness and understanding allows for better
management of these feelings and the capacity to avert the development of more
severe panic states. An ability to express anger in ways that feel safe is an
important development in the treatment. Increased assertiveness and the
capacity to communicate about conflicts in relationships improves quality of
life and reduces panic vulnerability.
Conducting Treatment with PFPP
Psychoanalysis
and psychodynamic psychotherapy have typically been thought to be indicated for
patients who enter treatment with a particular set of qualities that includes
being verbally skilled, psychologically minded, and curious about the origins
of their symptoms. Panic patients, however, with their tendency to experience conflicts
and affects as focused in their bodies, have limited verbal access to their
intrapsychic life and may be frightened to pursue the origins of their
problems. The author of this article and colleagues have found that patients
without these skills can obtain relief of symptoms from PFPP.34,35 A
case example illustrates some of the aspects of treatment with this approach.
Engaging the Patient
Several
factors enable PFPP to work as a short-term treatment or as an intervention
that can help people with little exposure to psychotherapy. This treatment
includes a component of psychoeducation, not only about panic disorder, but
also about the psychodynamic model and how it operates. In early sessions the
therapist focuses on exploring the circumstances and feelings preceding panic
onset. Patients become engaged with the treatment as they see the relationship
between their symptoms, the stresses preceding onset, the feelings surrounding
panic, and their developmental history.
Ms. A
was a 43-year-old married woman with two children who described the onset of
panic attacks 1 month prior to consultation. She presented with a symptom
picture that met criteria for panic disorder along with mild symptoms of
depression. She recalled a series of panic attacks just after leaving home for
college, but these had resolved spontaneously. At first Ms. A described her
panic as having emerged out of the blue. However, on exploration the therapist
learned that the initial panic attack occurred after an intense conflict with her
15-year-old daughter, the older of two siblings. Ms. A struggled with how to
manage her daughter and saw herself as unable to set limits. She viewed limit
setting as being “too mean.” Ms. A quickly grasped that her panic was likely related
to these conflicts and her difficulty managing them. She noted that she was
“not very assertive” and always had difficulty confronting others.
Following
this initial link of the onset of symptoms to family conflicts, Ms. A became
very curious about the sources of her problems. The discussion about her
daughter reminded her of her problems with her alcoholic father, who had a
severe temper problem. The therapist wondered if Ms. A was frightened of
expressing any disagreement with him.
Ms. A
responded: “Yes, I think I was scared of that. I am always trying to be nice to
people. I think that will get them to like me. But I am not sure that it is
really helping my daughter to do that.” In this instance, Ms. A was describing
reaction formation, in which her anger toward her daughter was converted into
becoming “too nice.” She then noted: “I realize I should be setting better
limits. Yesterday when I stood my ground with her I felt so much better.”
This
information, presented in the first two sessions of Ms. A’s treatment, already
provided valuable insights into the origins of her panic disorder. Such
triggers included the stress of the conflict with her daughter, difficulties
with her management of limit setting, and her fears of getting angry.
Transference
As
treatment progresses, the therapist has more opportunities to explore conflicts
as they emerge in transference. Oftentimes, these occur in the context of angry
feelings toward or separation fears from the therapist.
In a
later session, Ms. A complained about an incident with her daughter, and
referred to her as “difficult.” The therapist remarked that her view of her
child had partly to do with her own behavior, because she was aware that when
she set proper limits, her child responded. Although she did not state this during
the session, she experienced her therapist’s comments as suggesting she was a
bad mother, unwilling to take responsibility for her parenting. She became
anxious after the session. That evening she asked her husband to comfort her
but he responded that he had had a stressful day and wanted to read the paper.
Subsequently, she had the onset of a panic attack. The following session the
therapist and patient were able to determine that the patient was quite angry
at her therapist and husband, and her conflict about her anger triggered the
attack.
Working Through and Termination
Working
through involves identifying the presence of conflicts in different areas of
the patient’s life, allowing increased understanding of feelings and fantasies.
These areas include the patient’s relationship with the therapist and others as
well as the patient’s internal fantasy life. For example, Ms. A realized her
unassertiveness came from several sources, including fear of her temperamental
father, fear of her sister who was more aggressive and bolder, and identification
with her mother who was also unassertive and would not confront her father
about problems. Each of these instances helped to elucidate the patient’s worry
that asserting herself would lead to disruptions in her relationships. In fact,
she felt that being the “nice girl” maintained others’ interest in her.
Termination
provides an important opportunity for looking at these conflicts directly in
the relationship with the therapist. Anger at and fear of losing the therapist
will often intensify at this point, highlighting conflicts that emerged earlier
in the treatment. For example, in short-term (24-session) PFPP treatments,
patients were typically pleased about the progress they had made, but were
often able to express concern and frustration with the therapist about ending
treatment.34,35
Research on Psychodynamic Treatment of Panic
Disorder
As is
generally the case with psychodynamic psychotherapy or psychoanalysis, there
have been few systematic studies using manualized treatments for panic
disorder. Wiborg and Dahl36 conducted a randomized, controlled trial
of a manualized form of psychodynamic psychotherapy along with clomipramine
compared to clomipramine alone. The 3-month weekly psychotherapy combined with medication
reduced relapse at 18 months compared to patients treated with clomipramine
alone (9% vs. 91%).
An open
trial of PFPP was conducted with this approach consisting of 24 sessions over a
12-week period.34,35 Of 21 patients meeting Diagnostic and Statistical Manual of
Mental Disorders, Fourth Edition (DSM-IV)37
criteria for panic disorder, there were 4 dropouts. Sixteen of the remaining 17
patients had remission of panic and agoraphobia, as well as significant
quality-of-life improvements. These gains were maintained at 6-month follow up.
Notably, the 8 subjects who had also had comorbid major depressive disorder
experienced relief of these symptoms as well. Although not a randomized
controlled trial, the study suggested that PFPP can provide significant relief
of panic symptoms. A randomized controlled trial comparing PFPP to applied
relaxation therapy has been completed, but as of this writing the results have
not been published.
Conclusion
Given
that panic disorder remains a significant public health problem, it is
important to continue to develop approaches to its treatment. PFPP is a useful
alternative or adjunct to cognitive-behavioral therapy and/or medication. PFPP
addresses intrapsychic conflicts, defense mechanisms, developmental factors,
and transference issues not likely to be focused on in other treatments. Thus,
this approach may affect psychological factors that lead to vulnerability to
recurrence of panic or other difficulties associated with panic disorder. An
open trial demonstrated positive results. A completed placebo-controlled trial
should shed further light on the effectiveness of this treatmentmedical costs.
References
1. Otto MW, Tuby KS, Gould RA, McLean RY,
Pollack MH. An effect-size analysis of the relative efficacy and tolerability
of serotonin selective reuptake inhibitors for panic disorder. Am J Psychiatry.
2001;158(12):1989-1992.
2. Bakker A, van Balkom AJ, Spinhoven P.
SSRIs vs. TCAs in the treatment of panic disorder: a meta-analysis. Acta
Psychiatr Scand. 2002;106(3):163-167.
3. Wilkinson G, Balestrieri M, Ruggeri M,
Bellantuono C. Meta-analysis of double-blind placebo-controlled trials of
antidepressants and benzodiazepines for patients with panic disorder. Psychol
Med. 1991;21(4):991-998.
4. Barlow DH, Gorman JM, Shear MK, Woods
SW. Cognitive-behavioral therapy, imipramine, or their combination for panic
disorder: A randomized controlled trial. JAMA. 2000;283(19):2529-2536.
Errata in: JAMA. 2000;284(19):2450. JAMA. 2001;284(20):2597.
5. Craske MG, Brown TA, Barlow DH.
Behavioral treatment of panic: a two-year follow-up. Behav Ther.
1991;22(3):289-304.
6. Craske MG, DeCola JP, Sachs AD,
Pontillo DC. Panic control treatment for agoraphobia. J Anxiety Disord.
2003;17(3):321-333.
7. Marks IM, Swinson RP, Basoglu M, et
al. Alprazolam and exposure alone and combined in panic disorder with
agoraphobia. A controlled study in London and Toronto. Br J Psychiatry.
1993;162:776-787.
8. Shear MK, Maser JD. Standardized
assessment for panic disorder research. A conference report. Arch Gen
Psychiatry. 1994;51(5):346-354.
9. Mavissakalian M, Michelson L. Two-year
follow-up of exposure and imipramine treatment of agoraphobia. Am J
Psychiatry. 1986;143(9):1106-1112.
10. Nagy LM, Krystal JH, Woods SW, Charney
DS. Clinical and medication outcome after short-term alprazolam and behavioral
group treatment in panic disorder. 2.5 year naturalistic follow-up study. Arch
Gen Psychiatry. 1989;46(11):993-999.
11. Noyes R Jr, Garvey MJ, Cook BL.
Follow-up study of patients with panic disorder and agoraphobia with panic
attacks treated with tricyclic antidepressants. J Affect Disord.
1989;16(2-3):249-257.
12. Pollack MH, Otto MW, Tesar GE, Cohen
LS, Meltzer-Brody S, Rosenbaum JF. Long-term outcome after acute treatment with
alprazolam and clonazepam for panic disorder. J Clin Psychopharmacol.
1993;13(4):257-263.
13. Milrod B, Busch F. Long-term outcome of
panic disorder treatment. A review of the literature. J Nerv Ment Dis.
1996;184(12):723-730.
14. Vanelli M. Improving treatment response
in panic disorder. Primary Psychiatry. 2005;12(11):68-73.
15. Markowitz JS, Weissman MM, Ouellette R,
Lish JD, Klerman GL. Quality of life in panic disorder. Arch Gen Psychiatry.
1989;46(11):984-992.
16. Rubin HC, Rapaport MH, Levine B, et al.
Quality of well-being in panic disorder: the assessment of psychiatric and
general disability. J Affect Disord. 2000;57(1-3):217-221.
17. Katon W. Panic disorder: relationship
to high medical utilization, unexplained physical symptoms, and medical costs. J
Clin Psychiatry. 1996;57(suppl 10):11-18.
18. Swinson RP, Cox BJ, Woszczyna CB. Use
of medical services and treatment for panic disorder with agoraphobia and for
social phobia. CMAJ. 1992;147(6):878-883.
19. Fyer AJ, Liebowitz MR, Gorman JM, et
al. Discontinuation of alprazolam in panic patients. Am J Psychiatry.
1987;144(3):303-308.
20. O’Sullivan G, Marks I. Follow-up
studies of behavioral treatment of phobic and obsessive compulsive neurosis. Psych
Annals. 1991;21(6):368-373.
21. Busch FN, Cooper AM, Klerman GL,
Shapiro T, Shear MK. Neurophysiological, cognitive-behavioral and
psychoanalytic approaches to panic disorder: toward an integration. Psychoanalytic
Inquiry. 1991;11(3):316-332.
22. Shear MK, Cooper AM, Klerman GL, Busch
FN, Shapiro T. A psychodynamic model of panic disorder. Am J Psychiatry.
1993;150(6):859-866.
23. Milrod BL, Busch FN, Cooper AM, Shapiro
T. Manual of Panic-Focused Psychodynamic Psychotherapy. Washington, DC:
American Psychiatric Press; 1997.
24.
Breuer J, Freud S. Studies on hysteria (1895). In: Strachey J, trans and ed. The
Standard Edition of the Complete Psychological Works of Sigmund Freud. Vol
2. London, England: Hogarth Press; 1959:1-183.
25. Kleiner L, Marshall WL. The role of
interpersonal problems in the development of agoraphobia with panic attacks. J
Anxiety Disorders. 1987;1(4):313-323.
26. Freud S. The neuropsychoses of defence
(1894). In: Strachey J, trans and ed. The Standard Edition of the Complete
Psychological Works of Sigmund Freud. Vol 3. London, England: Hogarth
Press; 1959:45-61.
27. Busch FN, Shear MK, Cooper AM, Shapiro
T, Leon A. An empirical study of defense mechanisms in panic disorder. J
Nerv Ment Dis. 1995;183(5):299-303.
28. Parker G. Reported parental
characteristics of agoraphobics and social phobics. Br J Psychiatry.
1979;135:555-560.
29. Arrindell WA, Emmelkamp PM, Monsma A,
Brilman E. The role of perceived parental rearing practices in the aetiology of
phobic disorders: a controlled study. Br J Psychiatry. 1983;143:183-187.
30. Freud S: Inhibitions, symptoms and
anxiety (1926). In: Strachey J, trans and ed. The Standard Edition of the
Complete Psychological Works of Sigmund Freud. Vol 20. London, England:
Hogarth Press; 1959:77-174.
31. Kagan J, Reznick JS, Snidman N, et al.
Origins of panic disorder. In: Ballenger JC, ed. Neurobiology of Panic
Disorder. New York, NY: Wiley; 1990:71-87.
32. Fonagy P. Thinking about thinking: some
clinical and theoretical considerations in the treatment of a borderline
patient. Int J Psychoanal. 1991;72(pt 4):639-656.
33. Rudden MG, Milrod B, Aronson A, Target
M. Reflective functioning in panic disorder patients: clinical observations and
research design. Psychoanalytic Inquiry. In press.
34. Milrod B, Busch F, Leon AC, et al. A
pilot open trial of brief psychodynamic psychotherapy for panic disorder. J
Psychother Prac Res. 2001;10(4):239-245.
35. Milrod B, Busch F, Leon AC, et al. An
open trial of psychodynamic psychotherapy for panic disorder: a pilot study. Am
J Psychiatry. 2000;157(11):1878-1880.
36. Wiborg IM, Dahl AA. Does brief dynamic
psychotherapy reduce the relapse rate of panic disorder? Arch Gen Psychiatry.
1996;53(8):689-694.
37. Diagnostic and Statistical Manual of
Mental Disorders. 4th ed. Washington, DC: American Psychiatric Association;
1994.