Results from the STAR*D Study
October 20, 2006 |
Norman Sussman, MD, DFAPA |
Editor, Primary Psychiatry and Psychiatry Weekly, Professor
of Psychiatry, New York University School of Medicine
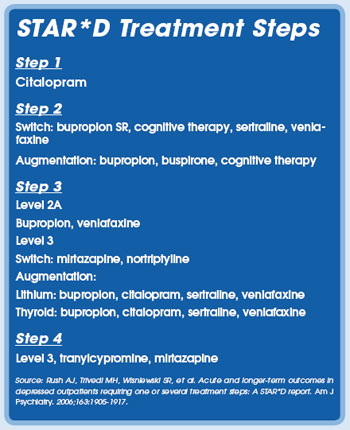
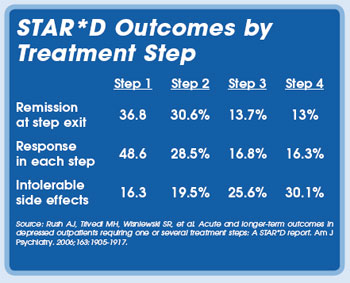
The long-awaited final results of the Sequenced Treatment Alternatives to Relieve Depression (STAR*D) study were published
in the November 2006 American Journal of Psychiatry. This trial, involving 3,671 patients, is the largest prospective
study ever conducted examining whether there are differences in response and remission rates with subsequent medication
trials. Results of the initial phase of the study found that only ~33% of patients achieved remission after up to 12 weeks
of citalopram. All patients were started on that drug. In each of the subsequent three phases of the trial, some patients
went into remission, but the likelihood of that outcome decreased. For example, initial remission rates on step one (citalopram
alone) were 36.8%. In step 2, an additional 30.6% of patients converted. At step 3, 13.7% converted, and after step 4,
13% went into remission. After four different regimens, the cumulative remission rate is 67%. The group that did not remit
until after four treatments, experienced the highest relapse rates. Only 4% remained well during the follow-up. Relapse
rates were lowest among those who went into remission during the earlier phases of the study. In the authors’ words, “when
more treatment steps are required, lower acute remission rates (especially in the third and fourth treatment steps) and
higher relapse rates during the follow-up phase are to be expected.”
Overall, in addition to the greater number of interventions used, characteristics that predicted worse outcome were greater
severity of the depression and concurrent psychiatric and medical conditions.
In many respects, the results of the study were disappointing, since they indicate that for most patients the first treatment
does not produce a full resolution of symptoms. Also, for some of the more problematic cases, sustained remission is less
assured. It serves to emphasize the importance of persistence in finding a treatment that works. The study did not look
at how patients who fail on antidepressants or other augmentation agents used in the study might respond if switched to
a mood stabilizer. There is considerable evidence that anticonvulsants and atypical neuroleptics may prove beneficial to
those who do not do well on antidepressant drugs.
Disclosure: Dr. Sussman has received honoraria from AstraZeneca, Bristol-Myers Squibb, and GlaxoSmithKline.