Print Friendly
Reducing the Risk of Late-Life Suicide Through Improved Depression Care
December 18, 2006
Gary J. Kennedy, MD
Professor, Psychiatry and Behavioral Sciences, Albert Einstein College of Medicine, Director, Division of Geriatric Psychiatry, Montefiore Medical Center
On September 14th, 2006, the United States Senate Special
Committee on Aging conducted a hearing titled, “Generation at Risk: Breaking
the Cycle of Senior Suicide,” in which chairman Smith called late-life suicide
an epidemic.1 Both Senator Smith and colleague Senator Kohl emphasized
the contribution of mental illness, specifically depression, as a preventable
cause of suicide among older Americans.1,2 They both
emphasized primary care settings as the logical avenue through which
improvements in depression care could lead to reduced rates of suicide in old
age. However, if late-life depression in primary care is the target, what
characterizes effective interventions, and how effective are they? What follows
is a review of studies which evaluated efforts to reduce suicidality through
improved depression care in primary practice settings.
Introduction
Since the introduction of
selective serotonin reuptake inhibitors (SSRIs), antidepressant prescriptions
increased by 400%, but suicidal deaths declined by only 3%.3 The
substitution of SSRIs, which are rarely lethal in overdose, for tricyclic
antidepressants, which are highly lethal, may be responsible for the decline.
Although antidepressant prescriptions provided by primary care physicians
(PCPs) have increased, the number of psychotherapy visits has declined. Moreover,
the largest increase in antidepressants has been among young adults, children,
and adolescents.4 Suicide rates have declined among older Americans,
but because of the increasing size of the aged population, the actual number of
suicidal deaths in old age has not.5 If depression is the major
cause of suicide in old age, simply increasing antidepressant prescriptions may
not be sufficient to sustain the decline in suicide rates.
Depression Care management
A more aggressive approach
to depression has emerged, incorporating principles of chronic disease
management similar to that employed to improve care and reduce hospitalizations
among people with diabetes or congestive heart failure. In primary care models
of chronic disease management, nursing personnel collaborate with physicians
and patients to improve adherence to evidence-based care. Specialist
consultation from cardiologists or endocrinologists is available, but the
majority of clinical interaction occurs between patient and nurse. For
depression, the collaboration integrates a depression care manager (DCM),
typically nurses with added psychiatric training, psychiatric social workers,
or psychologists. Psychiatric consultation is available, but again, the
majority of clinical interaction occurs between the patient and the Manager
rather than with physicians. Comprehensive geriatric evaluation management
clinics also employ interdisciplinary teams, including nurses, social workers,
and psychologists, to provide chronic disease management including depression
care.
Skultety and Zeiss6
found both comprehensive geriatric evaluation and the integrated models more
effective than routine care in reducing depression in late life. However because
the integrated models were designed specifically for depression and were more
likely to focus interventions on severe depression, the models and their
outcomes were difficult to compare. Gilbody and colleagues7 compared
costs and benefits of physician education, collaborative care, and case
management in studies of depression in primary practices. The authors found
uniformly superior outcomes for collaborative care and case management but no
benefit from education alone. However, incremental improvements in depression
care were associated with increments in costs. In summary, a collaborative,
interdisciplinary approach to depression in primary care settings is cost
effective but does not reduce the total costs of care. Two of the eight studies
reviewed by Skultety and Zeiss6 also attempted to reduce suicidality
and are examined in greater detail.
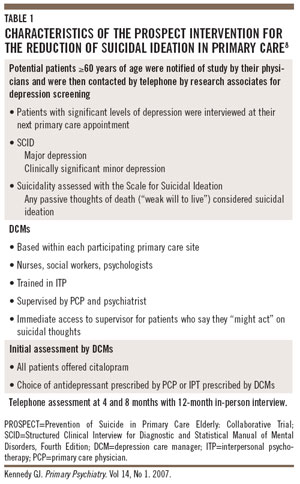
PROSPECT
The Prevention of Suicide
in Primary Care Elderly: Collaborative Trial (PROSPECT) integrated a DCM into
primary care sites.8 Details of the methodology appear in Table 1.
Through a screening process, patients with clinically significant levels of
depressive symptoms were assessed by telephone and received an in-person
interview with the Scale for Suicidal Ideation. Twelve percent of those
screened, or >500 people, expressed a significant level of depressive
symptoms. Two thirds of the sample exhibited major depressive disorder (MDD).
PROSPECT defined subjects with a score >0 on the Scale for Suicidal Ideation
as having suicidal ideas. As a result, the sample included people with “weak
desire to live today” as expressing suicidal ideation. This threshold was set
purposefully low in light of the finding by Brown and colleagues9
that psychiatric patients =55 years of age who scored =1 on the Scale for Suicidal
Ideation exhibited a 15.5-fold increased risk of suicide compared to those who
scored 0.
Among PROSPECT patients
who reported suicidal ideation at baseline, 66.7% of intervention patients were
free of suicidal ideation by 4 months compared to 58.7% of those receiving
routine care (P=.34). By
8 months, the difference between intervention and routine care groups was both
more substantial and significant (70.7% versus 43.9%, P=.005). However, by 12 months, the two groups were
nearly identical (68.7% versus 65.8%, P=.89).
Stated differently, after 12 months suicidal ideas among those receiving the
intervention had declined 12.9% points (from 29.4% to 16.5%) compared to a
decline of 3.0% points (from 20.1% to 17.1%) among the treatment as usual group
(P=.01). Among the 202 patients with minor
depression, intervention was superior to routine care only for the 23 with
suicidal ideation (P=.03).
Regarding the depression response (omnibus trend P=.003) and remission rates (omnibus trend P=.001), the patients receiving the intervention
experienced statistically superior outcomes over 1 year of observation.
However, only 54.8% met criteria for remission. Thus, nearly one third of
depressed patients continued to express suicidal ideation and slightly more
than half experienced a remission of depression.
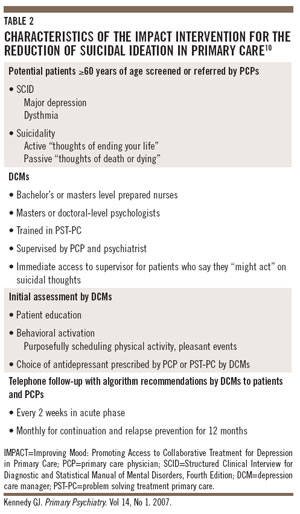
IMPACT Study
In the Improving Mood:
Promoting Access to Collaborative Treatment for Depression in Primary Care
(IMPACT) study which, like PROSPECT, integrated a DCM, 13.3% of 1,801 depressed
primary care patients randomized to routine care and 15.9% in the intervention
group expressed passive or active thoughts of suicide. Details of the IMPACT
intervention appear in Table 2. Patients in the intervention group exhibited
significantly lower rates of active suicidal ideation at 6 months (7.5% versus
12.1%) and at 12 months (9.8% versus 15.5%) following baseline. Even after the
DCMs were withdrawn, the beneficial effects remained significant for the
intervention group at 18 months (8.0% versus 13.3%) and 24 months (10.1% versus
13.9%). The intervention was also significantly more effective than routine
care in reducing passive thoughts of death at 6 months (27% versus 38%), 13
months (32% versus 51%), 18 months (38% versus 50%), and 24 months (41% versus
50%). In addition, among patients who received an emergent evaluation because
they could not assure the DCMs or non-clinician outcomes evaluators that they
would not act on suicidal impulses, significantly more were in the routine care
than intervention group (7.7% versus 4.3%).10
In summary, both PROSPECT
and IMPACT integrated specially trained mental health personnel into primary
care settings. Both studies monitored adherence to antidepressant guidelines,
providing advice to physicians and patients when deviations occurred. Psychotherapy
and psychiatric consultation were readily available. However, both depressive
symptoms and suicidal ideas remained in a sizeable minority of patients in both
studies despite their interventions. These studies demonstrate the extent to
which suicidality may be reduced when the effort is limited to sites of primary
care only.
Reducing Suicidality Beyond
Primary Care
Expanding the effort to
reduce suicidality with a more broadly deployed approach to depression would be
expected to provide added benefits. Paykel and colleagues’11 “Defeat
Depression Campaign” included pubic information efforts to reduce stigma and
promote treatment as well as updating physicians on advances in diagnosis and
treatment of depression. Suicide rates declined by 11.7%. A similar public
education effort in Australia titled “beyondblue” resulted in an increase in
public awareness.12 Suicide rates were reduced and antidepressant
prescriptions increased in the Island of Gotland through an intensive
educational program for PCPs.13 However, none of these programs
employed a comparison population such that the observed effects may have been
due to events not associated with the intervention.
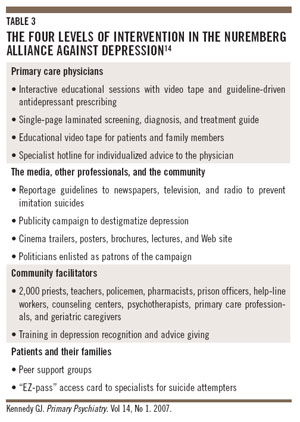
The Nuremberg alliance
against depression (NAD) to reduce suicidality study used a broadly based
multi-level intervention to compare suicidal deaths and suicide attempts over 2
years between Nuremberg and Wurzburg. As shown in Table 3, four levels of a
comprehensive community and clinical intervention were directed at the
population of Nuremberg while Wurzburg received observation only. The four
levels of intervention demonstrate an effort to saturate the environment with a
social marketing campaign to recognize and reduce depression and thereby
suicidality. The campaign was targeted at PCPs and patients and their families,
but also incorporated an array of communications media as well as
“facilitators” to serve as potential case sentinels and informal community
advisers for people who might be depressed. At both 12 and 24 months following
the intervention, rates of suicide declined in both cities, although the
reductions were statistically significant in neither. However, the decline in
suicide attempts was significantly and substantially greater from baseline to
12 months (approximately 18.3%) and baseline to 24 months (approximately 26.5%)
in Nuremberg but not in Wurzburg. The reductions in attempts were most
noticeable for highly lethal means (shooting, hanging, and jumping) and among
persons <70 years of age.14 Obviously, the advantage of a large-scale
population-based study is its capacity to count suicidal behaviors and not just
depressive symptoms. However, its size and design precluded the inclusion of
DCMs.
Similar to the NAD, the
Oregon Older Adult Suicide Prevention Plan seeks the broadest possible attack
on the elements of suicidal risk in late life.15 Table 4 is a
reduced list of the strategic objectives for Oregon’s clinical,
community-based, and public health interventions. The introduction of
integrated models of depression care into primary practice is but one element.
Yet, the evidence supporting the integration of DCMs is among the strongest,
and methods to sustain their presence in primary care beyond the
research-funded initiatives of PROSPECT and IMPACT are critical.
Paying for the Model
The challenge of paying
for the DCM arises largely from lack of adequate fee-for-service Medicare
procedure codes and other financial incentives within capitated systems of
care. However, reflecting on his experience with the IMPACT study, Jürgen Unützer,
director of the IMPACT Coordinating Center, noted that “under Medicare
Advantage there is actually a very strong incentive to document depression
diagnosis and treatment, and a well run depression care management program can
facilitate this and lead to significantly higher capitated payments for
depressed patients. This has been a major motivator for one of the largest
Medicare Advantage plans (offered by Kaiser Permanente) to roll an adapted
version of the IMPACT model out to over 10 large regional medical centers in
Southern California and they currently have over 20,000 patients in depression
care management.” (Personal communication, November 20, 2006.)
Within fee-for-service
settings, Medicare reimburses services such as psychiatric diagnostic interview,
follow-up medication management or psychotherapy with medication management,
and psychiatric consultation. However, psychotherapy without medication
management is subject to 50% co-pay, which is a substantial disincentive to
many patients unless they also have a medigap policy. Unützer added that “a
master’s level clinical nurse specialist who bills largely fee-for-service
insurance for IMPACT care delivered in two Duke [University Medical Center]
affiliated primary care clinics, covers the majority of her salary with
billings which include some direct billing to Medicare and some ‘incident to
physician’ billing.” (Personal
communication, November 20, 2006.)
However, DCM activities
not covered by Medicare include communications other than those which occur
directly, face-to-face with the patient. These include telephone monitoring of
patient needs as well as telephone consultation with the patient’s PCP or
psychiatrist. Thus, failure to reimburse for telephone communication is a
barrier to widespread integration of DCMs into primary care settings. The
failure is all the more problematic given findings from the Re-Engineering Systems
for Primary Care Treatment of Depression study which employed a DCM whose sole
contact with patients was via the telephone. Although not focused on older
adults, the telephone intervention in the context of psychiatric oversight and
specifically prepared PCPs was associated with a maintenance of minimal suicide
risk among patients with dysthymia or MDD.16
Both the President’s New
Freedom Commission on Mental Health17 and the National Business
Group on Health18 have made strong recommendations that public
(including federal) and private payers reimburse such evidence-based services.
Bachman and colleagues19 have proposed a number of funding
mechanisms and find the prospects of improved funding optimistic. Concerns for
the economic impact of parent care on younger adults in the work force add to
the incentive for improved geriatric mental health care.20
Other Issues
There are additional
issues relevant to detection and reduction of suicide risk among older adults.
First is the controversy over the extent to which passive thoughts of death as
assessed in PROPSECT and IMPACT predict risk of active suicidal ideation.21
In a study of patients with recurrent depressive disorder and either passive or
active suicidal ideation, Szanto and colleagues22 found depressed
patients with passive suicidal thoughts were as pessimistic about the future as
those with active thoughts but denied intent to harm themselves. As treatment
continued, active suicidal thoughts became passive before disappearing
entirely, suggesting a continuum of risk and the utility of questions for
passive thoughts of death.
The second issue relevant
to depression and suicidality in primary care is chronic pain. In a recent
review of pain and suicide, Tang and Crane23 noted that the risk of
suicidal death appeared to be at least doubled in chronic pain patients. The
prevalence of suicidal ideation was 20% among people with chronic pain, with 5%
to 14% reporting a prior suicide attempt. Eight risk factors were associated
with suicidality and chronic pain, including the type, intensity, and duration
of pain, and sleep-onset insomnia. Helplessness and hopelessness about pain,
the desire for escape from pain, and catastrophic self-assessments were also
associated. Coping by avoidance and deficits in problem-solving skills were
prominent psychological processes relevant to the understanding of suicidality
in chronic pain.
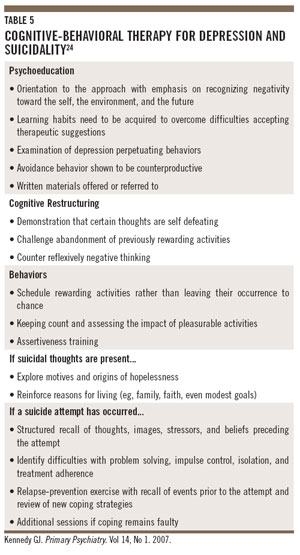
Interventions to
ameliorate the cognitive risk factors associated with depression, pain, and suicidality
have been developed. To site one example, Brown and colleagues24
randomized 120 patients following a suicide attempt to case management or
cognitive therapy plus case management. The cognitive therapy incorporated
preventative techniques specific to the suicidal impulse (Table 5). After 18
months, participants in the cognitive therapy arm were 50% less likely to have
re-attempted suicide and expressed less depression and hopelessness as well.
Nonetheless, there were no significant differences in rates of suicidal
ideation between the two groups. Moreover, 13 (24%) patients in cognitive
therapy and 23 (41%) in case management made at least one subsequent suicide
attempt.
Conclusion
The technology of
depression care has advanced substantially with important implications for the
reduction of suicidality in late life. The choice of medications singly, in
combination, and in sequence,25 modifications of psychotherapy,24
and the integration of mental health services within primary care provide an
evidence base upon which effective policy may be forged.19 Both
public and private concerns have mobilized in recognition of the need. However,
in order to continue the decline in late-life suicide rates, a national
strategy similar to the Oregon Plan or the Nuremberg Alliance may be necessary.
A social marketing campaign coupled with the financing of integrated models of
depression care seems the next logical step. With the science in hand,
anecdotes like Senator Smith’s public discussion of his son’s suicide or
Senator Reid’s disclosure of his father’s suicide26 may be necessary
to provide the impetus for change.
Disclosure: Dr. Kennedy has received research support or honoraria from AstraZeneca, Eli Lilly, Forest,
Janssen, and Pfizer.

References
1. Statement of
Chairman Gordon H. Smith, US Senate Special Committee on Aging. A generation at
Risk: Breaking the Cycle of Senior Suicide; Washington, DC; September 14, 2006.
Available at: http://aging.senate.gov/public/_files/hr164gs.pdf. Accessed
November 30, 2006.
2. Statement of
Senator Herb Kohl, US Senate Special Committee on Aging Hearing. A generation
at Risk: Breaking the Cycle of Senior Suicide; Washington, DC; September 14,
2006. Available at: http://aging.senate.gov/public/_files/hr164hk.pdf. Accessed
November 30, 2006.
3. Mann JJ, Apter A,
Bertolote J, et al. Suicide prevention strategies: a systematic review. JAMA.
2005;294(16):2064-2074.
4. McKeown RE, Cuffe
SP, Schulz RM. US suicide rates by age group, 1970-2002: an examination of
recent trends. Am J Public Health. 2006;96(10):1744-1751.
5. Kennedy GJ. Will more antidepressants mean fewer
suicides in late life? Primary Psychiatry. 2005;12(1):26-29.
6. Skultety KM, Zeiss
A. The treatment of depression in older adults in the primary care setting: an
evidence-based review. Health Psychol. 2006;25(6):665-674.
7. Gilbody S, Bower
P, Whitty P. Costs and consequences of enhanced care for depression; Systematic
review of randomized economic evaluations. Br J Psychiatry.
2006;189:297-308.
8. Bruce ML, Ten Have
TR, Reynolds CF 3rd, et al. Reducing suicidal ideation and depressive symptoms
in depressed older primary care patients: a randomized controlled trial. JAMA.
2004;291(9):1081-1091.
9. Brown GK, Beck AT,
Steer RA, Grisham JR. Risk factors for suicide in psychiatric outpatients: a
20-year prospective study. J Consult Clin Psychol. 2000;68(3):371-377.
10. Unützer J, Tang L,
Oishi S, et al. Reducing suicidal ideation in depressed older primary care
patients. J Am Geriatric Soc. 2006;54(10):1550-1556.
11. Paykel ES, Tylee A,
Wright A, Priest RG, Rix S, Hart D. The Defeat Depression Campaign: psychiatry
in the public arena. Am J Psychiatry. 1997;154(6 suppl):59-65.
12. Jorm AF,
Christensen H, Griffiths KM. The impact of beyondblue: the national depression
initiative on the Australian public’s recognition of depression and beliefs
about treatment. Aust N Z J Psychiatry. 2005;39(4):248-254.
13. Rutz W, von
Knorring L, Walinder J, Wistedt B. Effect of an educational program for general
practitioners on Gotland on the pattern of prescription of psychotropic drugs. Acta
Psychaitr Scand. 1990;82(6):399-403.
14. Hegerl U, Althaus
D, Schmidtke A, Niklewski G. The alliance against depression: 2-year evaluation
of a community-based intervention to reduce suicidality. Psychol Med.
2006;36(9):1225-1233.
15. Oregon Older
Adult Suicide Prevention Plan. Available at:
http://egov.oregon.gov/DHS/ph/ipe/esp/docs/plan.pdf. Accessed November 29,
2006.
16. Schulberg HC, Lee
PW, Bruce ML, et al. Suicidal ideation and risk levels among primary care
patients with uncomplicated depression. Ann Fam Med. 2005;3(6):523-528.
17. President’s New
Freedom Commission on Mental Health. Available at: www.mentalhealthcommission.gov/reports/reports.htm.
Accessed November 29, 2006.
18. National Business
Group on Health. Available at:
www.businessgrouphealth.org/prevention/depression.cfm. Accessed November 29,
2006.
19. Bachman J, Pincus
HA, Houtsinger JK, Unützer J. Funding mechanisms for depression care
management: opportunities and challenges. Gen Hosp Psychiatry.
2006;28(4):278-288.
20. MetLife Mature
Market Institute. Caregiving Cost Study. Available at:
www.metlife.com/WPSAssets/17239064071161116019V1FCaregiverCostStudy7.11.06.pdf.
Accessed November 30, 2006.
21. Raue PJ, Brown EL,
Meyers BS, Schulberg HC, Bruce ML. Does every allusion to possible suicide
require the same response? J Fam Pract. 2006;55(7):605-612.
22. Szanto K, Reynolds
CF, Frank E, et al. Suicide in elderly depressed patients: Is active vs.
passive suicidal ideation a clinically valid distinction? Am J Geriatr
Psychiatry. 1996;4(3):197-207.
23. Tang NK, Crane C.
Suicidality in chronic pain: a review of the prevalence, risk factors and
psychological links. Psychol Med. 2006;36(5):575-586.
24. Brown GK, Ten Have
T, Henriques GR, Xie SX, Hollander JE, Beck AT. Cognitive therapy for the
prevention of suicide attempts: a randomized controlled trial. JAMA.
2005;294(5):563-570.
25. Kennedy GJ. The
Sequenced Treatment Alternatives to Relieve Depression studies: how applicable
are the results for older adults? Primary Psychiatry. 2006;13(11):33-36.
26. Congressional Press
Releases. Reid calls for a national suicide prevention strategy. May 6, 1997.
FDCHeMedia, Inc. No. 97-095.