Print Friendly
The Highs & Lows of Bipolar Disorder
Robert M.A. Hirschfeld, MD
Dr. Hirschfeld is Professor and Chair, Department of Psychiatry and Behavioral Sciences, University of Texas Medical Branch
Dr. Robert Hirschfeld has focused on mood disorders for the entirety of his professional career. He became particularly interested in bipolar disorder and unipolar depression while serving as Chief of the scientific advisory board for the National Depressive and Manic Depressive Association, where he worked closely with patients and patients’ families who helped and advocated for people with depression and bipolar disorder. Dr. Hirschfeld has made tremendous contributions toward the classification, diagnosis, and treatment of bipolar and other mood disorders.
Diagnosis
Dr. Hirschfeld stresses that bipolar disorder and unipolar depression are not on the same spectrum of diseases. Bipolar disorder refers to those who have highs—while depression commonly alternates with the highs attendant to bipolar disorder, it isn’t an essential part of the diagnosis, and different treatments are often required for bipolar disorder and depressive disorders. Some patients will present with hyperthymia—they’re characterized by their social intrusiveness, and they often have increased energy, pressured speech, and unbounded enthusiasm. However, these patients experience no lows.
It is the periodic highs—mania in bipolar I and hypomania in bipolar II—that distinguish the condition, and they must be the focus of the diagnosis. It can be difficult for a clinician to identify these highs, or even find evidence for them, Dr. Hirschfeld points out, because patients who alternate between depression and mania usually present when they’re down, not when they’re up. A complete history, including interviews with family members and significant others, is essential when diagnosing patients presenting with depression so as to identify or rule out bipolar disorder.
Indeed, Dr. Hirschfeld believes bipolar disorder to be significantly under-diagnosed. He created the Mood Disorder Questionnaire (MDQ) (Table 1) to help clinicians accurately diagnose bipolar disorder, but emphasizes that, “if you’re just going to ask a couple of questions, ask your patient: Do you have mood swings and/or unnatural highs? and do these ever get you into trouble?” While everyone experiences some minor mood swings and natural ups and downs in energy level, it’s the impairment of function resultant from being up that’s essential in diagnosing mania and/or hypomania, and thus bipolar disorder.
Pharmacotherapy
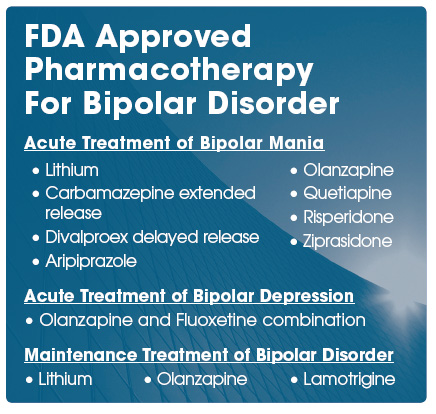
Antidepressants are being overprescribed to patients with bipolar disorder, Dr. Hirschfeld believes. This is sometimes due to misdiagnosis, and sometimes it’s due to misconceptions regarding treating bipolar disorder. “In general,” Dr. Hirschfeld says, “it’s much wiser to start out with lithium or mood stabilizers or some of the atypicals: quetiapine, for instance, has shown to be very useful in treatment of both depression and bipolar disorder.” If prescribed without a concurrent mood stabilizer, traditional antidepressants such as SSRIs can destabilize patients with bipolar disorder, and can even precipitate manic episodes. “They are sometimes necessary,” Dr. Hirschfeld allows, “but it’s not where you start.”
The atypicals, a group of drugs with dopaminergic action and substantially lower risk of extraparametal signs and tardive dyskenisia, have been very successful in trials, according to Dr. Hirschfeld. However, he cautions, while the data show effectiveness for a year or longer, “we want to see what happens over several years before we really can be confident that they should be used equally with lithium, divalproex, and so on.”
Conclusion
Clinicians must stay on their toes when diagnosing patients presenting with depression. Taking a full history and keeping an eye out for the tell-tale signs of bipolar disorder can prevent misdiagnosis and decreases the chances of prescribing the wrong pharmacotherapy. Lithium, lamotrigine, and divalproex are tried and true treatments for bipolar disorder, but the atypical antidepressants are showing a great deal of promise as well.